Ciencias Psicológicas; v19(2)
July-December 2025
10.22235/cp.v19i2.4460
Original Articles
What can we learn to increase vaccination in Latin America: Factors associated with COVID-19 vaccination
Qué podemos aprender para aumentar la vacunación en Latinoamérica: factores asociados a la vacunación contra la COVID-19
O que podemos aprender para aumentar a vacinação na América Latina: fatores associados à vacinação contra a COVID-19
Susana Torres1, ORCID 0000-0001-5393-1296
Juan Pablo Román-Calderón2, ORCID 0000-0002-4352-8513
Mariantonia Lemos3, ORCID 0000-0002-9131-4704
1 Universidad EAFIT, Colombia
2 Universidad EAFIT, Colombia
3 Universidad EAFIT; iCARE Study Team, Colombia, [email protected]
Abstract:
Background: Even though vaccination may serve to effectively overcome the COVID-19 pandemic, vaccine hesitancy is still prevalent and affected by different variables. This research is intended to understand which variables influence the likelihood of an individual getting a COVID-19 vaccine in a sample from Latin America, applying the COM-B model. Method: 368 individuals from Latin America answered a self-administered, cross-sectional survey from the iCARE study. Survey data began in March 2020 using convenience snowball sampling (globally) and parallel representative sampling in targeted countries. Results: A structural equation model showed that knowing that getting vaccinated will help protect others, wanting to contribute to high vaccination rates among the population to achieve herd immunity, and believing that getting vaccinated would reduce personal worries and anxiety predict the likelihood of an individual getting vaccinated. This shows that in this sample, motivators are more salient than capabilities and opportunities regarding vaccination uptake. Conclusions: Campaigns to reduce vaccine hesitancy need to highlight the prosocial factors of getting vaccinated and increase vulnerability and risk perceptions regarding the disease.
Keywords: vaccination; COVID-19; Latin America; COM-B model.
Resumen:
Introducción: A pesar de que la vacunación es un comportamiento de protección que puede permitir superar la pandemia por el COVID-19, la reticencia a vacunarse es aún prevalente para esta y otras enfermedades. Esta investigación busca comprender cuáles variables influencian la probabilidad de vacunarse en una muestra en Latinoamérica aplicando el modelo COM-B. Método: 368 personas de Latinoamérica respondieron una encuesta autoreportada y transversal como parte del estudio iCARE. La recolección inició en marzo de 2020 usando un muestreo por conveniencia en bola de nieve (a nivel mundial) y un muestreo representativo paralelo en países seleccionados. Resultados: Un modelo de ecuaciones estructurales mostró que saber que vacunarse ayudará a proteger a otros, querer contribuir a unos mayores índices de vacunación para alcanzar la inmunidad de rebaño y creer que vacunarse reducirá las preocupaciones propias y síntomas de ansiedad son variables que predicen la probabilidad de vacunarse. Esto muestra que las motivaciones en esta muestra son más relevantes que las capacidades y oportunidades en lo que a este comportamiento refiere. Conclusiones: Las campañas para reducir la reticencia para vacunarse necesitan resaltar los factores psicosociales para vacunarse e incrementar la vulnerabilidad y el riesgo percibidos respecto a la enfermedad.
Palabras clave: vacunación; COVID-19; Latinoamérica; modelo COM-B.
Resumo:
Introdução: Embora a vacinação seja uma medida de proteção que pode permitir superar a pandemia da COVID-19, a hesitação em vacinar-se ainda é prevalente para esta e outras doenças. Esta pesquisa busca compreender quais variáveis influenciam a probabilidade de se vacinar em uma amostra na América Latina, aplicando o modelo COM-B. Método: 368 pessoas da América Latina responderam a uma pesquisa autorrelatada e transversal como parte do estudo iCARE. A coleta iniciou-se em março de 2020 utilizando amostragem por conveniência em bola de neve (em nível mundial) e uma amostragem representativa paralela em países selecionados. Resultados: Um modelo de equações estruturais mostrou que saber que vacinar-se ajudará a proteger outras pessoas, querer contribuir para maiores índices de vacinação a fim de alcançar a imunidade de rebanho e acreditar que vacinar-se reduzirá as próprias preocupações e sintomas de ansiedade são variáveis que predizem a probabilidade de vacinar-se. Isso mostra que, nesta amostra, as motivações são mais relevantes do que as capacidades e oportunidades no que diz respeito a esse comportamento. Conclusões: As campanhas para reduzir a hesitação em vacinar-se precisam destacar os fatores psicossociais para a vacinação e aumentar a vulnerabilidade e o risco percebidos em relação à doença.
Palavras-chave: vacinação; COVID-19; América Latina; modelo COM-B.
Received: 03/02/2025
Accepted: 29/08/2025
Vaccine hesitancy is a complex and context-specific behavior that involves a “delay in acceptance or refusal of vaccination despite the availability of vaccination services” (MacDonald et al., 2015, p. 4163). This has been a historical global concern (Tankwanchi et al., 2022) for various viral diseases such as Zika (Searles et al., 2023), dengue (Shafie et al., 2023), Human Papillomavirus (HPV) (Díaz et al., 2025), and others (Guzman-Holst et al., 2020; Matos et al., 2022). However, the COVID-19 pandemic highlighted the impact that different viral infections have on global health (Cankat et al., 2023) and emphasized the importance of creating appropriate strategies to increase vaccination rates. These strategies are crucial for mitigating the spread of the virus and achieving herd immunity as vaccine hesitancy could impair efforts to reach this goal (Bhopal & Nielsen, 2021; Kaur & Gupta, 2020; MacDonald et al., 2015; Orensteina & Ahmedb, 2017).
Research has demonstrated significant variations in vaccine hesitancy and uptake levels across countries for both COVID-19 (Bacon et al., 2021; Bates et al., 2022; Stojanovic et al., 2021) and other diseases (Guzman-Holst et al., 2020; Matos et al., 2022; Searles et al., 2023; Shafie et al., 2023). Notably, during the COVID-19 pandemic, Latin America emerged as one of the most severely impacted regions: the cases and mortality rates were exacerbated by misinformation (Dror et al., 2020) and structural challenges like poverty, corruption, inequality, and inadequate healthcare systems (Burki, 2020; Debbag et al., 2025; Pablos-Méndez et al., 2020; Urrunaga-Pastor et al., 2021). In addition, distrust in the vaccine itself (Lapo-Talledo et al., 2023) or in authorities stemming from corruption and various socioeconomic factors hindered the establishment of effective campaigns to improve vaccination rates (Burki, 2020; Eureka-Putri-Taju & Saadah, 2023; Pablos-Méndez et al., 2020).
To address these challenges, it is essential to understand the behavioral responses towards vaccination uptake. This can be achieved through theoretical frameworks such as the COM-B model. The COM-B model applies a broad perspective to comprehend behavior determinants, including individual and context factors. It posits that behavior occurs when capability (abilities that increase the probability of change), opportunity (social and environmental facilitators of change) and motivation (factors that increase the desire to change) are in place (Michie et al., 2011). In the case of vaccination, insufficient knowledge about COVID-19 was associated with uncertainty about getting vaccinated (Paul et al., 2021; Ruiz & Bell, 2021). However, it has also been pointed out that information and knowledge are not enough to increase immunization uptake, as vaccination decisions are often guided by heuristics, biases, emotions, and attitudes that cannot be changed solely through information provision (Giese et al., 2023; Habersaat & Jackson, 2020).
Moreover, significant barriers to vaccination persist, which encompass attitudes and motivations regarding health and taking preventive measures (Dror et al., 2020; Guzman-Holst et al., 2020). For instance, people with higher health concerns, both personal (Blank et al., 2012; Brewer et al., 2007; Stojanovic et al., 2021) and for others (Betsch et al., 2013; Böhm & Betsch, 2022; Stojanovic et al., 2021), are less likely to report vaccine hesitancy. However, the significance of certain variables may vary across populations. While some researchers have found that age (Murphy et al., 2021), sex (Sallam, 2021), and trust in the government or health professionals (Blank et al., 2012; d’Alessandro et al., 2012; Debbag et al., 2025; Murphy et al., 2021; Urrunaga-Pastor et al., 2021) are significant predictors of vaccination intent, other studies did not confirm these relations (Dror et al., 2020; Paul et al., 2021; Pogue et al., 2020).
Furthermore, although the main challenges regarding the COVID-19 vaccine emerged between 2020 and 2022 and the virus is no longer considered a global emergency, research on this topic remains important for two reasons. First, the vast amount of research arising from the need to understand vaccination intent can help generate strategies to promote immunization for other diseases that still affect various countries in Latin America; especially considering that vaccination uptake is associated with reduced disease burden (Moore et al., 2023; Qin et al., 2022). Second, there are ongoing clinical, social, and economic concerns associated with currently circulating variants of SARS-CoV-2, especially in Latin America, where there is a higher risk of complications and death due to new virus variants compared to other regions (Castilla et al., 2021; La Rotta et al., 2023). According to the World Health Organization (WHO, 2022), outbreaks of infectious diseases are increasingly frequent, and we might face the risk of new diseases emerging, and new or known diseases turning into pandemics. Consequently, the scientific community agrees on the need to develop more effective next-generation vaccines (Cankat et al., 2023), and, equally importantly, to create effective behavioral campaigns that increase vaccination uptake (Giese et al., 2023; WHO, 2022). In summary, research on the way people adhere to public and health policies, specifically regarding vaccination, is a foresight strategy that enable us to be better prepared for future health challenges.
Considering these arguments, one effective approach to designing and implementing campaigns to improve vaccination uptake is by identifying context-specific issues and critical barriers within populations (Giese et al., 2023; Habersaat & Jackson, 2020; Matos et al., 2022). Correspondingly, the International COVID-19 Awareness and Responses Evaluation (iCARE) Study (https://icare.mbmc-cmcm.ca/) is an international multi-wave cross-sectional observational cohort study of public awareness, attitudes, and responses to public health policies implemented to reduce the spread of COVID-19 around the world (Bacon et al., 2021). The iCARE survey was launched in March 2020 during the first phase of the COVID-19 pandemic. Its primary objective was to comprehend how people coped and behaved in such a critical situation; a scenario that we might encounter again in the future.
According to the above, the aim of this study was to identify the way the dimensions of the COM-B model influence the likelihood of getting a COVID-19 vaccine in a sample from Latin America.
Method
Participants
The data analyzed in this paper corresponds to the complete data survey of Latin America iCARE study participants from March 27, 2020 to June 15, 2021. This study was launched in March 2020 using convenience snowball sampling (globally) and parallel representative sampling in targeted countries. The study is led by the Montreal Behavioural Medicine Centre (MBMC: www.mbmc-cmcm.ca) in collaboration with a team of 200 international collaborators from 42 countries. The sample analyzed included 363 adult participants. The mean age of the participants was 40.54 years (SD = 14.43). The majority were women (73.6 %) and had a college or university degree (46.1 %), as shown in Table 1.
Table 1: Characteristics of the simple
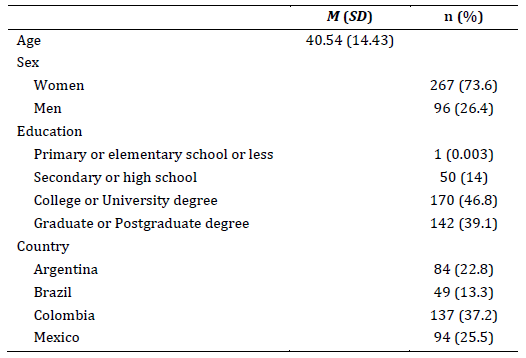
Note: M: Mean; SD: Standard deviation.
Instrument and variables
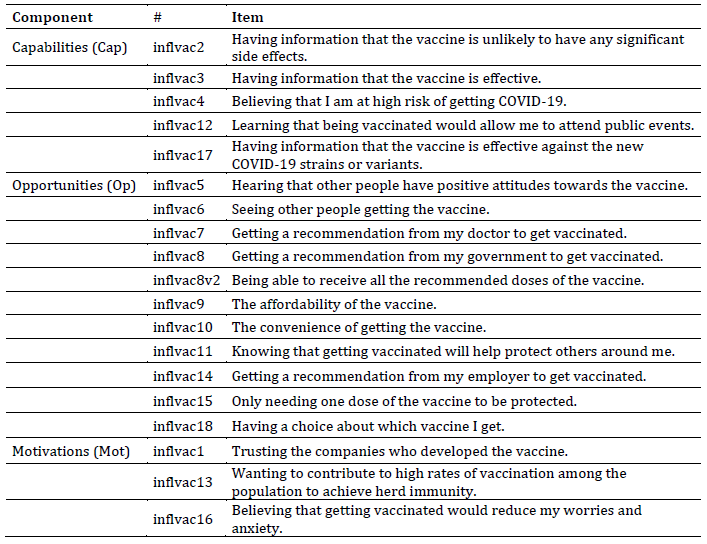
The survey used in the iCARE study was available in 34 languages. Translations of the questionnaire were done by the researcher team who validate that the translations were faithful to the original. This questionnaire assessed a wide variety of domains as detailed by Bacon et al. (2021). The likelihood of getting a COVID-19 vaccine was assessed through the following item: “if a vaccine for COVID-19 were available today, what is the likelihood that you would get vaccinated?” These items were answered using a Likert scale (1: To a great extent, 2: Somewhat, 3: Very little, 4: Not at all, 5: I do not know/I prefer not to answer). Also, for this research, we focused on independent variables that potentially influence vaccination decisions. These variables were categorized according to the COM-B model: capabilities (awareness of prevention measures and the ability to implement them), opportunities (social and environmental facilitators for behavior adoption), and motivations (beliefs about the personal relevance and importance of preventive measures). A detailed explanation of these variables is provided in Table 2.
Table 2: Items according to the COM-B model
Procedure
The survey was distributed using a link that redirects to a webpage. The first step that the participant had to take is choosing the language. After this, the informed consent was presented, and the participant should accept it in order to complete the questionnaire. Answering the questionnaire took around 20 to 25 minutes. It has received REB approval from the Comité d’éthique de recherche du CIUSSS-NIM (Centre intégré universitaire de santé et de services sociaux du Nord-de-l’île-de-Montréal), approval #: 2020-2099 / 25-03-2020.
Statistical analysis
The authors used the Mplus statistical package v.8.8 (Muthén & Muthén, 2017) to analyze the quantitative data. The Exploratory Structural Equation modeling (ESEM) approach makes it possible to explore the psychometric properties of the scales and test relationships with given covariates. Therefore, an ESEM was selected to explore whether the items of the iCARE survey reflected the constructs of the COM-B model and to simultaneously test whether the variables in the model affected the probability of getting vaccinated.
To assess the fit of the specified model, general rules were adopted for the CFI, RMSEA and SRMR coefficients (Hu & Bentler, 1999). Additionally, they evaluated the fit of the ESEM model using the chi-square (χ2) index. A non-significant chi-square suggests a good fit for the evaluated models. To cope with some violations of the normality assumption, the researchers chose the maximum likelihood with robust standard errors (MLR) estimator. They used the CF-Varimax rotation method and examined the residual correlations to detect possible issues of a local misfit. The factor loadings of the items were evaluated considering a critical value of .40. The reliability of the COM factors was assessed by examining the omega coefficient. Usual rules of thumb were considered to this end (new measures should have reliability estimates above .70 (Nunnally, 1978). Finally, as some scholars found that age (Murphy et al., 2021) and sex (Sallam, 2021) affect the probability of getting vaccinated, the authors controlled for these variables.
Results
Descriptive analyses indicated generally low self-reported likelihood of vaccination, with higher endorsement of social influence factors (e.g., hearing positive attitudes from others, seeing others vaccinated) compared to knowledge-based or altruistic motivations. Structural equation modeling further showed that motivation was the strongest predictor of vaccination likelihood (β = .56, p < .001), whereas capability and opportunity were moderately interrelated but had weaker direct associations with vaccination intention. Overall, the findings suggest that social and motivational factors play a more prominent role than informational or altruistic considerations in shaping vaccination decisions within this sample.
In pursuing a more profound understanding of these results, the descriptive statistics of the items included in the model and the probability of being vaccinated are presented in Table 3. Overall, the likelihood of getting vaccinated was relatively low (M = 1.31, SD = 0.69, range = 1–4). Among the motivational factors, hearing that other people have positive attitudes toward the vaccine (M = 2.14, SD = 1.07) and seeing others getting vaccinated (M = 2.02, SD = 1.09) were rated higher than most other items, suggesting that social influence may play an important role in shaping vaccination intentions. In contrast, capability-related items such as having information about vaccine effectiveness (M = 1.23, SD = 0.05) or knowing that vaccination helps protect others (M = 1.15, SD = 0.44) received the lowest scores, indicating limited confidence in informational or altruistic drivers. Opportunity-related items, such as trust in the companies that developed the vaccine (M = 1.60, SD = 0.80) and believing that vaccination would reduce worries and anxiety (M = 1.85, SD = 1.03), fell in the mid-range.
Table 3: Descriptive statistics of the items
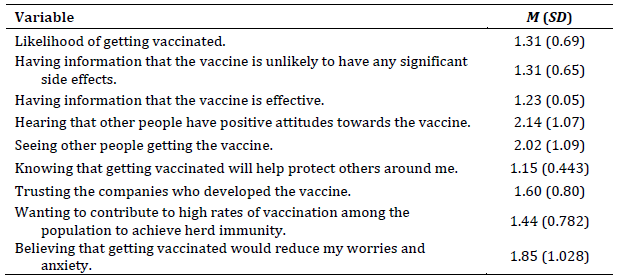
Note: M: Mean; SD: Standard deviation.
Structural analysis
The researchers ran an initial ESEM with the items of the iCARE survey mentioned above. Only complete data from the respondents were used in these analyses. Although the model provided acceptable results in some of the goodness of fit indexes, other coefficients suggested differently (χ2 = (63, N = 312) = 133.58, p = .00; CFI = .92; RMSEA = .06; SRMR = .04). Moreover, some items had low factor loadings in all factors (inflvac 4, inflvac8, inflvac 10, inflvac 12). After deleting the items that did not reach the criteria, the authors retained a total of eight items (57 % of the original items) which loaded in the COM-B theoretical factors. The skewness and kurtosis of the remaining items did not comply with the recommended rule of thumb (> -2; > 2). As mentioned above, this justified the use of the MLR estimator. The factor loadings and residual variances of the retained items are presented in Figure 1. The re-specified model (Figure 1) obtained satisfactory goodness of fit results (χ2 = (12, N = 363) = 15.97, p = .19; CFI = .99; RMSEA = .03; SRMR = .02). The correlations between capabilities, opportunities and motivations are below .80, suggesting discriminant validity of the scales. These positive and significant correlations also support the theoretical associations between the factors of the COM-B model.
Figure 1: Re-specified ESEM model
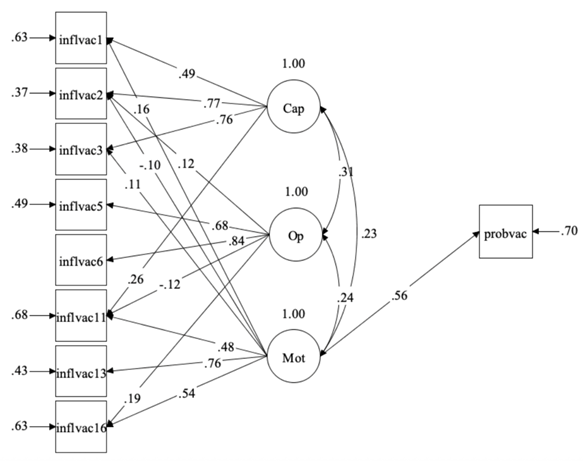
Notes: N = 368; Estimator: MLR; Rotation: CF-Varimax (oblique); Factor variances fixed to 1 as a default in the ESEM approach. All parameters were significant at the p <.01 level, except for p -> inflvac1, inflvac2 and Mot -> inflvac1, inflvac2, and inflvac3 significant at the p < .05.
The cross-loadings below .40 also suggest discriminant validity of the scales. Furthermore, the factor loadings above .40 on the COM-B theoretical factors are evidence of convergent validity (Figure 1). Concerning this new aggregation to the iCARE items, the results indicate that the capabilities and opportunities measures are reliable operationalizations of the COM-B factors (ωCap = .82 95 % CI [0.73, 0.90]; ωOp = .79 95 % CI [0.72, 0.86]; ωMot =.65 95 % CI [0.58, 0.72]. As motivations obtained a relative low reliability score, although acceptable under certain circumstances (Bates et al., 2022), the researchers investigated if deleting one of the items would increase the reliability of the scale. However, motivations omega values remained equal (eliminating inflvac11) or decreased (deleting inflvac13 or inflvac16).
As for the effect of the COM-B variables on the probability of getting vaccinated, the model explains 30 % (p = 0.00) of the variance of that outcome. In addition, the results of the study indicate that only motivations exerts a positive significant effect (Figure 1). This effect remained significant despite the insertion of the control variables into the model. It is noteworthy that none of the control variables exerted a significant effect on the probability of getting vaccinated (βage = -0.02, p = .61; βsex = 0.01, p = .78; βeducation = -0.001, p = .98).
Discussion
Vaccine acceptance, hesitancy and uptake can be understood through different lenses such as contextual, individual and vaccine specific (Ramonfaur et al., 2024). This study aimed to shed light on the social, environmental, and individual variables that influence the likelihood of getting a COVID-19 vaccine in a sample from Latin America to learn which variables are important to promote vaccination in future pandemics. These analyses reveal how the items were grouped according to the COM-B model, and they indicate that capabilities and opportunities are not crucial in vaccination uptake. However, it is important to understand that having the opportunity to have access to vaccines is the first step in a new pandemic. However, when you need to generate the motivation to increase the uptake of the vaccine, knowing that getting vaccinated will help protect others, that it will contribute to reaching high vaccination rates among the population to, in turn, achieve herd immunity, and believing that it will reduce individuals’ worries and anxiety, are better predictors of the likelihood of getting vaccinated than capabilities and opportunities.
The analyses revealed that both knowing that vaccination helps protect others and contributes to achieving herd immunity were associated with a higher probability of getting the vaccine. Consistent with previous research, vaccination provides both personal and social benefits (Betsch et al., 2013; Böhm & Betsch, 2022; Urrunaga-Pastor et al., 2021), which explains why individuals with higher health concerns for others are significantly less likely to report vaccine hesitancy (Böhm & Betsch, 2022; Caycho-Rodríguez et al., 2022; d’Alessandro et al., 2012; Stojanovic et al., 2021). Additionally, identifying as a part of a group (d’Alessandro et al., 2012) and having a sense of social responsibility influence vaccination decisions (Herry et al., 2023). Regarding social responsibility influencing vaccine behavior, studies analyzing vaccine acceptance in health workers shed light on the importance of health workers promoting vaccination amongst patients since they are seen as a trustworthy source in terms of health (Pandher & Bilszta, 2023; Rivera et al., 2023). An example of the influence of health workers on patients' decisions regarding vaccines is showcased when even hesitant breast cancer patients said they would be willing to get vaccinated if their oncologist suggested it (Ramonfaur et al., 2024)
These findings align with Latin American cultures, where collectivism influences vaccination uptake for various diseases (Askarian et al., 2022; Guzman-Holst et al., 2020; Salazar-Fernández et al., 2022; Urrunaga-Pastor et al., 2021). In the case of COVID-19, a study conducted across 13 Latin-American countries found that a high concern about infecting others significantly predict intention to be vaccinated for COVID-19 (Caycho-Rodríguez et al., 2022).
Furthermore, when analyzed collectively, social opportunity emerged as a more relevant factor for vaccination uptake in this sample compared to environmental opportunity, which other studies have found to be more significant (Askarian et al., 2022; Salazar-Fernández et al., 2022; Stojanovic et al., 2021). The results in this study suggest that alluding to social benefits appears to be more influential than emphasizing individual risks of not getting vaccinated. This is evidenced by the fact that believing oneself to be at high individual risk of contracting COVID-19 was not a significant predictor in the model. In addition to social opportunity, various studies demonstrate that opinions of family and friends have a substantial influence on COVID-19 vaccination decisions in Latin America, positive experiences from significant others or vaccination as a family tradition are facilitators for vaccine acceptance (Rivera et al., 2023; Roberti et al., 2024; Salazar-Fernández et al., 2022). A thematic analysis of barriers and facilitators of vaccination in Latin America revealed various social variables as facilitators in vaccine behavior, one of the most relevant findings was vaccination being perceived as an act of love and responsible caretaking of children, it was also recognized as a requirement to be admitted in academic and labor settings; therefore viewed as important to access these opportunities (Roberti et al., 2024). Nevertheless, even though social opportunity plays a significant role in vaccination uptake, it's important to note that emphasizing indirect social benefits can unintentionally foster free-riding behavior. Therefore, it is crucial to implement strategies to counteract this potential negative outcome (Betsch et al., 2013; Böhm & Betsch, 2022).
These results also expose that allude to emotions is crucial for changing behavior (Habersaat & Jackson, 2020; Rosenstock et al., 1988). Contrary to other research (Paul et al., 2021; Ruiz & Bell, 2021), building knowledge about vaccines mechanisms and how they were developed did not predict the likelihood of getting vaccinated in this sample. Furthermore, vaccine literacy does not necessarily mean lower vaccine fear or higher vaccine acceptance as it was shown in a study with health volunteers in Thailand (Siewchaisakul et al., 2022). However, believing that getting vaccinated would reduce worries and anxiety did. These results align with the Health Belief Model (Rosenstock et al., 1988), which posits that perceiving being threatened by the disease and identifying benefits from the treatment increase the likelihood of adopting healthy behavior. Several studies have demonstrated that fear of severe COVID-19 infection is negatively related to vaccine hesitancy (Dror et al., 2020; Ruiz & Bell, 2021; Urrunaga-Pastor et al., 2021). Conversely, an identity of being healthy and immune from infection reduces the perceived need to get vaccinated (Rubinstein et al., 2015). Additionally, factors such as vaccine fear, risk, susceptibility, and severity perceptions are associated with vaccination behavior in general (Brewer et al., 2007; Qin et al., 2022; Rodrigues et al., 2023) and specifically for COVID-19 (Caycho-Rodríguez et al., 2022). Interestingly, personally knowing someone who became severely ill or died from COVID-19, or being related to people who tested positive, did not predict a higher likelihood of getting vaccinated. Pogue et al. (2020) obtained similar results and suggested that the ubiquitous impact of the COVID-19 outbreak may have diluting the effects of personal experiences.
While previous studies have found associations between sociodemographic variables and COVID-19 vaccines uptake (Lazarus et al., 2021; Murphy et al., 2021; Paul et al., 2021; Urrunaga-Pastor et al., 2021), this study did not identify significant differences in vaccination likelihood related to sex or other demographic variables. In this sample, demographic factors appear to be less salient than motivational factors, which align with results reported by Pogue et al. (2020). Consistent with other studies focusing on the region (Bates et al., 2022; Eureka-Putri-Taju & Saadah, 2023; Lapo-Talledo et al., 2023), this research revealed that structural barriers were not significant for eluding vaccination. This phenomenon may be attributed to the implementation of regional vaccination campaigns that emphasise interpersonal communication people-centered (Bates et al., 2022) and empowerment approaches (Chan et al., 2022; Díaz et al., 2025), and messages from credible medical sources (Argote et al., 2021). This shows that such campaigns have successfully targeted important factors in the region, which should be considered when developing strategies to promote positive responses to vaccines in future scenarios since stringent government mandates, which have the potential to precipitate unintended consequences, given the correlation between individuals' perceptions of government pandemic management and their acceptance of vaccines (Debbag et al., 2025).
Considering these findings, it is essential to align vaccination initiatives with the unique characteristics of specific regions. In this regard, the COM-B model can serve as a valuable resource for identifying the behavioral dimensions that should be targeted in order to reduce vaccine hesitancy. In this population, the implementation of emotional strategies and the promotion of social benefits derived from the vaccine could constitute a pragmatic approach to designing vaccination campaigns. Furthermore, experts and researchers propose several theoretical and empirical recommendations aligned with the results of this study. For instance, some behavioral communicational tools that can improve the effectiveness of campaigns based on social opportunity include: (a) increasing the perception that without the vaccine, the chances of infecting someone close to you are higher; (b) emphasizing that infection may occur without one realizing it; and (c) evoking the feeling of being indispensable to achieve herd immunity (Contreras-Arrieta et al., 2023). Furthermore, designing interventions and messages that rise susceptibility and severity of the disease; as well as providing information on how the vaccine effectively and safely prevents the infection —thereby, reducing fear and anxiety of testing positive, is recommended as emotions are crucial in eliciting vaccination uptake (Contreras-Arrieta et al., 2023; Rivera et al., 2023).
Before concluding, it is important to highlight some limitations of this study. Generalizations based on these results should be taken with caution due to the convenience sampling methodology being used. On the other hand, the sample was not proportional, so differences between countries cannot be established. Moreover, the questionnaire measures intention, which might overestimate actual behaviour, and using a Likert scale might lead to central tendency bias. However, it is important to note that iCARE study is one of the biggest studies that was launched in the middle of the pandemic and that implies that the results are not affected by memory biases because the data were collected in the middle of the pandemic. Additionally, these results support the importance of addressing vaccine hesitancy by highlighting the prosocial factors of getting vaccinated or as a form of collective care and increasing susceptibility and severity perceptions. Such approaches may also be effective in promoting vaccination uptake both for COVID-19 and other viruses.
In conclusion, this study provides valuable insights about the factors influencing COVID-19 vaccine uptake in Latin America based on the COM-B model as a theoretical framework. These findings reveal that, in this sample, social opportunity and automatic motivation are stronger predictors of vaccination likelihood than capabilities or environmental opportunity. The significance of prosocial motivations, such as protecting others and contributing to herd immunity, aligns with the collectivist cultural values prevalent in Latin America. Moreover, the crucial role of emotional factors, specifically the belief that vaccination will reduce anxiety and worries, underscores the importance of addressing emotional components in vaccination campaigns in Latin America. It is important to note that these findings do not deny the importance of capabilities and environmental opportunity in vaccination uptake. Rather, they highlight the relative prominence of social and motivational factors in this particular context. This underscores the complex interplay of factors influencing vaccination decisions and emphasizes the need for multifaceted approaches in addressing vaccine uptake.
Additionally, these findings enhance our comprehension of vaccine intent in the region. As we face the ongoing challenges posed by COVID-19 and prepare for potential future health crisis and pandemics, this research offers a solid foundation for developing more effective, targeted and culturally sensitive health interventions that can improve vaccination rates and, ultimately, protect population health across Latin America.
References
Argote, P., Barham, E., Daly, S. Z., Gerez, J. E., Marshall, J., & Pocasangre, O. (2021). The shot, the message, and the messenger: COVID-19 vaccine acceptance in Latin America. Npj Vaccines, 6(1). https://doi.org/10.1038/s41541-021-00380-x
Askarian, M., Semenov, A., Llopis, F., Rubulotta, F., Dragovac, G., Pshenichnaya, N., Assadian, O., & Ruch, Y. (2022). The COVID-19 vaccination acceptance/hesitancy rate and its determinants among healthcare workers of 91 countries: A multicenrer cross-sectional study. EXCLI Journal, 21, 93-103. https://doi.org/https://doi.org/10.17179/excli2021-4439
Bacon, S. L., Lavoie, K. L., Boyle, J., Stojanovic, J., & Joyal-Desmarais, K. (2021). International assessment of the link between COVID-19 related attitudes, concerns and behaviours in relation to public health policies: Optimising policy strategies to improve health, economic and quality of life outcomes (the iCARE Study). BMJ Open, 11(3). https://doi.org/10.1136/bmjopen-2020-046127
Bates, B. R., Villegas-Botero, A., Costales, J. A., Moncayo, A. L., Tami, A., Carvajal, A., & Grijalva, M. J. (2022). COVID-19 Vaccine Hesitancy in Three Latin American Countries: Reasons Given for Not Becoming Vaccinated in Colombia, Ecuador, and Venezuela. Health Communication, 37(12), 1465-1475. https://doi.org/https://doi.org/10.1080/10410236.2022.2035943
Betsch, C., Böhm, R., & Korn, L. (2013). Inviting free-riders or appealing to prosocial behavior? Game-theoretical reflections on communicating herd immunity in vaccine advocacy. Health Psychology, 32(9), 978-985. https://doi.org/10.1037/a0031590
Bhopal, S., & Nielsen, M. (2021). Vaccine hesitancy in low- And middle-income countries: Potential implications for the COVID-19 response. Archives of Disease in Childhood, 106(2), 113–114. https://doi.org/10.1136/archdischild-2020-318988
Blank, P. R., Bonnelye, G., Ducastel, A., & Szucs, T. D. (2012). Attitudes of the General Public and General Practitioners in Five Countries towards Pandemic and Seasonal Influenza Vaccines during Season 2009/2010. PLoS ONE, 7(10), 1-8. https://doi.org/10.1371/journal.pone.0045450
Böhm, R., & Betsch, C. (2022). Prosocial vaccination. Current Opinion in Psychology, 43, 307-311. https://doi.org/10.1016/j.copsyc.2021.08.010
Brewer, N. T., Chapman, G. B., Gibbons, F. X., Gerrard, M., McCaul, K. D., & Weinstein, N. D. (2007). Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychology, 26(2), 136-145. https://doi.org/10.1037/0278-6133.26.2.136
Burki, T. (2020). COVID-19 in Latin America. The Lancet. Infectious Diseases, 20(5), 547-548. https://doi.org/10.1016/S1473-3099(20)30303-0
Cankat, S., Demael, M. U., & Swadling, L. (2023). In search of a pan-coronavirus vaccine: next-generation vaccine design and immune mechanisms. Cellular and Molecular Immunology, 21(2), 103–118. https://doi.org/10.1038/s41423-023-01116-8
Castilla, J., Guevara, M., Miqueleiz, A., Baigorria, F., Ibero-Esparza, C., Navascués, A., Trobajo-Sanmartín, C., Martínez-Baz, I., Casado, I., Burgui, C., & Ezpeleta, C. (2021). Risk factors of infection, hospitalization and death from SARS-CoV-2: A population-based cohort study. Journal of Clinical Medicine, 10(12), 1-13. https://doi.org/10.3390/jcm10122608
Caycho-Rodríguez, T., Valencia, P. D., Vilca, L. W., Carbajal-León, C., Vivanco-Vidal, A., Saroli-Araníbar, D., Reyes-Bossio, M., White, M., Rojas-Jara, C., Polanco-Carrasco, R., Gallegos, M., Cervigni, M., Martino, P., Palacios, D. A., Moreta-Herrera, R., Samaniego-Pinho, A., Rivera, M. E. L., Ferrari, I. F., Flores-Mendoza, C., … Intimayta-Escalante, C. (2022). Prevalence and Predictors of Intention to be Vaccinated Against COVID-19 in Thirteen Latin American and Caribbean Countries. Trends in Psychology, 31, 865-889. https://doi.org/10.1007/s43076-022-00170-x
Chan, I. L., Mowson, R., Pedro, J., Roberti, J., Contreras, M., & Velandia-gonzález, M. (2022). Promoting immunization equity in Latin America and the Caribbean: Case studies, lessons learned, and their implication for COVID-19 vaccine equity. Vaccine, 40(13), 1977-1986. https://doi.org/10.1016/j.vaccine.2022.02.051
Contreras-Arrieta, S., Murrain, H., Vallejo, B. H., López, L. A. C., Hernández, F., Velasco, N., Garzón, J. S., Restrepo, S., & Varela, A. R. (2023). Vaccination against COVID-19 in Bogotá - Colombia: lessons and strategies in health pedagogy, risk communication and community participation, using behavioral sciences. Infectio, 27(3), 173-182. https://doi.org/10.22354/24223794.1142
d’Alessandro, E., Hubert, D., Launay, O., Bassinet, L., Lortholary, O., Jaffre, Y., & Sermet-Gaudelus, I. (2012). Determinants of refusal of A/H1N1 pandemic vaccination in a high risk population: A qualitative approach. PLoS ONE, 7(4). https://doi.org/10.1371/journal.pone.0034054
Debbag, R., Gallo, J., Ávila-Agüero, M. L., Beltran, C., Brea-Del Castillo, J., Puentes, A., & Enrique, S. (2025). Rebuilding vaccine confidence in Latin America and the Caribbean: strategies for the post-pandemic era. Expert Review of Vaccines, 24(1), 615–623. https://doi.org/10.1080/14760584.2025.2527327
Díaz, L., Villarreal, D. M., Márquez, K., & Scartascini, C. (2025). Combating Vaccine Hesitancy: The Case of HPV Vaccination. https://doi.org/https://doi.org/10.18235/0013410
Dror, A. A., Eisenbach, N., Taiber, S., Morozov, N. G., Mizrachi, M., Zigron, A., Srouji, S., & Sela, E. (2020). Vaccine hesitancy: the next challenge in the fight against COVID-19. European Journal of Epidemiology, 35(8), 775-779. https://doi.org/10.1007/s10654-020-00671-y
Eureka-Putri-Taju, A., & Saadah, K. (2023). Corruption in Mexico and Vaccine Refusal. KnE Social Sciences, 8(3), 11-21. https://doi.org/10.18502/kss.v8i3.12812
Giese, H., Neth, H., Wegwarth, O., Gaissmaier, W., & Stok, F. M. (2023). How to convince the vaccine-hesitant? An ease-of-access nudge, but not risk-related information increased Covid vaccination-related behaviors in the unvaccinated. Applied Psychology: Health and Well-Being, 16(1), 198-215. https://doi.org/10.1111/aphw.12479
Guzman-Holst, A., DeAntonio, R., Prado-Cohrs, D., & Juliao, P. (2020). Barriers to vaccination in Latin America: A systematic literature review. Vaccine, 38(3), 470–481. https://doi.org/10.1016/j.vaccine.2019.10.088
Habersaat, K. B., & Jackson, C. (2020). Understanding vaccine acceptance and demand—and ways to increase them. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz, 63(1), 32-39. https://doi.org/10.1007/s00103-019-03063-0
Herry, A. M., Greaves, D., Smith, P., Toledo, N. A., Wildman, A., Wildman, T., Browne, R., Chen, M., Jones, M., & Aymat, S. (2023). Facilitators of and barriers to COVID-19 vaccination in Grenada: a qualitative study. Revista Panamericana de Salud Pública, 47, 1. https://doi.org/10.26633/rpsp.2023.44
Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1-55. https://doi.org/https://doi.org/10.1080/10705519909540118
Kaur, S. P., & Gupta, V. (2020). COVID-19 Vaccine: A comprehensive status report. Virus Research, 288. https://doi.org/10.1016/j.virusres.2020.198114
La Rotta, J., Escobar, O., Ávila-Aguero, M. L., Torres, J. P., Sini de Almeida, R., Morales, G. del C., & Srivastava, A. (2023). COVID-19 in Latin America: A Snapshot in Time and the Road Ahead. Infectious Diseases and Therapy, 12(2), 389-410. https://doi.org/10.1007/s40121-022-00748-z
Lapo-Talledo, G. J., Talledo-Delgado, J. A., Portalanza, D., Ballaz, S., & Siteneski, A. (2023). Analysis of Socio-demographic, Economic and Individual Reasons for COVID-19 Vaccination Hesitancy in Ecuador: A Nationwide Longitudinal Study. Journal of Community Health, 48(3), 467-479. https://doi.org/10.1007/s10900-023-01188-7
Lazarus, J. V., Ratzan, S. C., Palayew, A., Gostin, L. O., Larson, H. J., Rabin, K., Kimball, S., & El-Mohandes, A. (2021). A global survey of potential acceptance of a COVID-19 vaccine. Nature Medicine, 27(2), 225–228. https://doi.org/10.1038/s41591-020-1124-9
MacDonald, N. E., Eskola, J., Liang, X., Chaudhuri, M., Dube, E., Gellin, B., Goldstein, S., Larson, H., Manzo, M. L., Reingold, A., Tshering, K., Zhou, Y., Duclos, P., Guirguis, S., Hickler, B., & Schuster, M. (2015). Vaccine hesitancy: Definition, scope and determinants. Vaccine, 33(34), 4161–4164. https://doi.org/10.1016/j.vaccine.2015.04.036
Matos, C. C. de S. A., Gonçalves, B. A., & Couto, M. T. (2022). Vaccine hesitancy in the global south: Towards a critical perspective on global health. Global Public Health, 17(6), 1087–1098. https://doi.org/10.1080/17441692.2021.1912138
Michie, S., van Stralen, M. M., & West, R. (2011). The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science, 6(1). https://doi.org/10.1186/1748-5908-6-42
Moore, S., Hill, E. M., Dyson, L., Tildesley, M. J., & Keeling, M. J. (2023). Retrospectively modeling the effects of increased global vaccine sharing on the COVID-19 pandemic. Nature Medicine, 28(11), 2416-2423. https://doi.org/10.1038/s41591-022-02064-y
Murphy, J., Vallières, F., Bentall, R. P., Shevlin, M., Mcbride, O., Hartman, T. K., Mckay, R., Bennett, K., Mason, L., Gibson-miller, J., Levita, L., Martinez, A. P., Stocks, T. V. A., Karatzias, T., & Hyland, P. (2021). Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nature Communications, 12(29). https://doi.org/https://doi.org/10.1038/s41467-020-20226-9
Muthén, L. K., & Muthén, B. O. (2017). Mplus User’s Guide(8th ed.) [Software].
Nunnally, J. C. (1978). Psychometric theory. McGrawHill.
Orensteina, W. A., & Ahmedb, R. (2017). Simply put: Vaccination saves lives. Proceedings of the National Academy of Sciences of the United States of America, 114(16), 4031–4033. https://doi.org/10.1073/pnas.1704507114
Pablos-Méndez, A., Vega, J., Aranguren, F. P., Tabish, H., & Raviglione, M. C. (2020). Covid-19 in Latin America. The BMJ, 370, 369-370. https://doi.org/10.1136/bmj.m2939
Pandher, R., & Bilszta, J. L. C. (2023). Novel COVID-19 vaccine hesitancy and acceptance, and associated factors, amongst medical students: a scoping review. Medical Education Online, 28(1). https://doi.org/10.1080/10872981.2023.2175620
Paul, E., Steptoe, A., & Fancourt, D. (2021). Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. The Lancet regional health. Europe, 1, 100012. https://doi.org/10.1016/j.lanepe.2020.100012
Pogue, K., Jensen, J. L., Stancil, C. K., Ferguson, D. G., Hughes, S. J., Mello, E. J., Burgess, R., Berges, B. K., Quaye, A., & Poole, B. D. (2020). Influences on attitudes regarding potential covid‐19 vaccination in the united states. Vaccines, 8(4), 1-14. https://doi.org/10.3390/vaccines8040582
Qin, C., Wang, R., Tao, L., Liu, M., & Liu, J. (2022). Acceptance of a Third Dose of COVID-19 Vaccine and Associated Factors in China Based on Health Belief Model: A National Cross-Sectional Study. Vaccines, 10(1), 1-13. https://doi.org/10.3390/vaccines10010089
Ramonfaur, D., Limaye, R. J., Hinojosa-González, D. E., Barrera, F. J., Rodríguez-Gómez, G. P., & Castillo-Salgado, C. (2024). COVID-19 vaccine hesitancy prevalence in Mexico: A systematic review and metanalysis. Vaccine, 18, 100488. https://doi.org/10.1016/j.jvacx.2024.100488
Rivera, T., Brustrom, J., Vera Antelo, M., Puertas, E. B., Rhoda, D. A., & Velandia-Gonzalez, M. (2023). Understanding COVID-19 Vaccine Acceptance among Latin American Health Workers: Implications for Designing Interventions. Vaccines, 11(9), 1-15. https://doi.org/10.3390/vaccines11091471
Roberti, J., Ini, N., Belizan, M., & Alonso, J. P. (2024). Barriers and facilitators to vaccination in Latin America: a thematic synthesis of qualitative studies. Cadernos de Saude Publica, 40(6). https://doi.org/10.1590/0102-311XEN165023
Rodrigues, E. S., Mendes, E. D. T., & Nucci, L. B. (2023). Parental Justifications for Not Vaccinating Children or Adolescents against Human Papillomavirus (HPV). Vaccines, 11(3), 506. https://doi.org/10.3390/vaccines11030506
Rosenstock, I. M., Strecher, V. J., & Becker, M. H. (1988). Social learning theory and the health belief model. Health Education Quarterly, 15(2), 175-183.
Rubinstein, H., Marcu, A., Yardley, L., & Michie, S. (2015). Public preferences for vaccination and antiviral medicines under different pandemic flu outbreak scenarios. BMC Public Health, 15(1), 1-13. https://doi.org/10.1186/s12889-015-1541-8
Ruiz, J. B., & Bell, R. A. (2021). Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine, 39(7), 1080-1086. https://doi.org/10.1016/j.vaccine.2021.01.010
Salazar-Fernández, C., Baeza-Rivera, M. J., Villanueva, M., Bautista, J. A. P., Navarro, R. M., & Pino, M. (2022). Predictors of COVID-19 Vaccine Intention: Evidence from Chile, Mexico, and Colombia. Vaccines, 10(7). https://doi.org/10.3390/vaccines10071129
Sallam, M. (2021). Covid-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines, 9(2), 1-15. https://doi.org/10.3390/vaccines9020160
Searles, M., Jose Ronquillo Mora, Y., Carlo, L., Heydari, N., Takyiwaa, Y., Borbor-Cordova, M. J., & Campagna, C. D. (2023). Zika virus knowledge and vaccine acceptance among undergraduate students in Guayaquil, Ecuador. Vaccine: X, 13, 100258. https://doi.org/10.1016/j.jvacx.2022.100258
Shafie, A. A., Moreira, E. D., Di Pasquale, A., Demuth, D., & Yin, J. Y. S. (2023). Knowledge, Attitudes and Practices toward Dengue Fever, Vector Control, and Vaccine Acceptance Among the General Population in Countries from Latin America and Asia Pacific: A Cross-Sectional Study (GEMKAP). Vaccines, 11(3), 575. https://doi.org/10.3390/vaccines11030575
Siewchaisakul, P., Sarakarn, P., Nanthanangkul, S., Longkul, J., Boonchieng, W., & Wungrath, J. (2022). Role of literacy, fear and hesitancy on acceptance of COVID-19 vaccine among village health volunteers in Thailand. PLoS ONE, 17(6), e0270023. https://doi.org/10.1371/journal.pone.0270023
Stojanovic, J., Boucher, V. G., Gagne, M., Gupta, S., Joyal-Desmarais, K., Paduano, S., Aburub, A. S., Sheinfeld Gorin, S. N., Kassianos, A. P., Ribeiro, P. A. B., Bacon, S. L., & Lavoie, K. L. (2021). Global trends and correlates of covid-19 vaccination hesitancy: Findings from the icare study. Vaccines, 9(6), 1-13. https://doi.org/10.3390/vaccines9060661
Tankwanchi, A. S., Jaca, A., Ndlambe, A. M., Zantsi, Z. P., Bowman, B., Garrison, M. M., Larson, H. J., Vermund, S. H., & Wiysonge, C. S. (2022). Non-COVID-19 vaccine hesitancy among migrant populations worldwide: a scoping review of the literature, 2000-2020. Expert Review of Vaccines, 21(9), 1269-1287. https://doi.org/10.1080/14760584.2022.2084075
Urrunaga-Pastor, D., Bendezu-Quispe, G., Herrera-Añazco, P., Uyen-Cateriano, A., Toro-Huamanchumo, C. J., Rodriguez-Morales, A. J., Hernandez, A. V., & Benites-Zapata, V. A. (2021). Cross-sectional analysis of COVID-19 vaccine intention, perceptions and hesitancy across Latin America and the Caribbean. Travel Medicine and Infectious Disease, 41. https://doi.org/10.1016/j.tmaid.2021.102059
World Health Organization. (2022). Imagining the future of pandemics and epidemics.
Data availability: The dataset supporting the results of this study is not available.
Funding: iCARE is supported by the Canadian Institutes of Health Research (CIHR: MM1-174903; MS3-173099; SMC-151518), the Canada Research Chairs Program (950-232522, Chair holder: Dr. Kim L. Lavoie), the Fonds de recherche du Québec Santé (FRQ-S: 251618 and 34757), the Fonds de Recherche du Québec Société et Culture (FRQSC: 2019-SE1-252541), and the Ministère de l'Économie et de l’Innovation du Québec (2020-2022-COVID-19-PSOv2a-51754). Study sponsors had no role in the design of the database and data collection.
Conflict of interest: The authors declare that they have no conflicts of interest.
How to cite: Torres, S., Román-Calderón, J. P., & Lemos, M. (2025). What can we learn to increase vaccination in Latin America: Factors associated with COVID-19 vaccination. Ciencias Psicológicas, 19(2), e-4460. https://doi.org/10.22235/cp.v19i2.4460
Authors’ contribution (CRediT Taxonomy): 1. Conceptualization; 2. Data curation; 3. Formal Analysis; 4. Funding acquisition; 5. Investigation; 6. Methodology; 7. Project administration; 8. Resources; 9. Software; 10. Supervision; 11. Validation; 12. Visualization; 13. Writing: original draft; 14. Writing: review & editing.
S. T. has contributed in 1, 5, 13, 14; J. P. R.-C. in 2, 3, 6, 9; M. L. in 1, 2, 5, 6, 7, 8, 10, 11, 12, 14. The last author is a members of de *iCARE Study Team.
* iCARE Study Team: Lead investigators: Kim L. Lavoie, PhD, University of Quebec at Montreal (UQAM) and CIUSSS-NIM, Canada; Simon L. Bacon, PhD, Concordia University and CIUSSS-NIM, Canada. Colaborators (in alphabetical order): Argentina: Nora Granana, PhD, Hospital Durand; Australia: Jacqueline Boyle, PhD, Monash University; Margie Danchin, PhD, Melbourne Medical School; Joanne Enticott, PhD, Monash University; Jessica Kaufman, PhD, Murdoch Children's Research Institute; Austria: Alexandra Kautzky-Willer, MD, Medizinische Universität Wien; Brazil: Eduardo Caputo, PhD, Universidade Federal de Pelotas; CANADA: Mohamad Baydoun, PhD, University of Regina; Andrea Gershon, PhD, Sunnybrook Research Institute; Ariane Bélanger-Gravel, PhD, Université Laval; Tavis Campbell, PhD, University of Calgary; Linda Carlson, PhD, University of Calgary; Kim Corace, PhD, University of Ottawa; Rubee Dev, PhD, University of British Colombia; Olivier Drouin, MD, CHU Sainte-Justine/Université de Montréal; Gary Garber, PhD, University of Ottawa/Public Health Ontario; Samir Gupta, MD, University of Toronto; Catherine Herba PhD, UQAM; Jack Jedwab, PhD, Canadian Institute for Identities and Migration and the Association for Canadian Studies; Keven Joyal-Desmarais, PhD, Concordia University; Joanne Liu, PhD, McGill University; Sandra Pelaez, PhD, Universitéde Montréal; Paul Poirier, MD, Université Laval; Justin Presseau, PhD, University of Ottawa; Eli Puterman, PhD, University of British Columbia; Joshua Rash, PhD, Memorial University; Johanne Saint-Charles, PhD, UQAM; Jovana Stojanovic, PhD, Concordia University; Michael Spivock, PhD, Shared Services Canada; Geneviève Szczepanik, PhD, MBMC; Michael Vallis, PhD, Dalhousie University; Vincent Gosselin Boucher, PhD, The University of British Columbia, Faculty of Eduction, School of Kinesiology; Claudia Trudel-Fitzgerald, PhD, Department of Psychology, Université du Québec à Trois-Rivières; Tamara Cohen, PhD, University of British Colombia; Alysha Deslippe, PhD, University of British Colombia. Colombia: Mariantonia Lemos-Hoyos, PhD, Universidad EAFIT; Cyprus: Angelos Kassianos, PhD, University of Cyprus; FRANCE: Gregory Ninot, PhD, Université de Montpellier; Mathieu Beraneck, PhD, Université Paris Cité, CNRS; Germany: Beate Ditzen, PhD, Heidelberg University; Greece: Theodora Skoura, PhD, Aretaieio Hospital Athens University; India: Delfin Lovelina Francis MDS (PhD) Saveetha Dental College and Hospitals, SIMATS; Ireland: Hannah Durand, PhD, University of Stirling; Oonagh Meade, PhD, University of Galway; Gerry Molloy, PhD, University of Galway; Chris Noone, PhD, University of Galway; Italy: Stefania Paduano, PhD, University of Modena and Reggio Emilia; Valeria Raparelli, MD PhD, University of Ferrara; Kenya: Hildah Oburu, PhD, University of Nairobi. Nepal: Niroj Bhandari, MBBS, Institute for Implementation Science and Health. Saudi Arabia: Abu Zeeshan Bari, PhD, Taibah University; Slovakia: Iveta Nagyova, PhD, PJ Safarik University - UPJS; Switzerland: Susanne Fischer, PhD, University of Zurich; Turkey: Ceprail Şimşek, MD Health Science University; UK: Joanne Hart, PhD, Manchester University; Lucie Byrne-Davis, PhD, University of Manchester; Nicola Paine, PhD, Loughborough University; Susan Michie, PhD, University College London; USA: Michele Okun, PhD, University of Colorado; Sherri Sheinfeld Gorin, PhD, University of Michigan; Johannes Thrul, PhD, John Hopkins University; Abebaw Yohannes, PhD, Azusa Pacific University. Students (in alphabetical order): Australia: Shrinkhala Dawadi, MSc, Monash University; Kushan Ranakombu, PhD, Monash University; Brazil: Daisuke Hayashi Neto, Msc, Unicamp; Canada: Frédérique Deslauriers, BA, UQAM and CIUSSS-NIM; Amandine Gagnon-Hébert, BA, UQAM and CIUSSS-NIM; Mahrukh Jamil, BA, Concordia University and CIUSSS-NIM; Camille Léger, BSc, UQAM and CIUSSS-NIM; Callum MacLeay, BA, UQAM and CIUSSS-NIM; Ariany Marques Vieira, MSc, Concordia University and CIUSSS-NIM; Sarah O’Connor, BA, Université Laval; Zackary van Allen, PhD, University of Ottawa; Colombia: Susana Torres, MSc, Universidad EAFIT. Community Participants: Canada: Sophie Duval, MSc; Johanne O’Malley; Katherine Séguin, BA; Kyle Warkentin; India: Sarah Tanishka Nethan.
Scientific editor in-charge: Dr. Cecilia Cracco.
Ciencias Psicológicas; v19(2)
July-December 2025
10.22235/cp.v19i2.4460
Original Articles