Ciencias Psicológicas; v19(2)
July-December 2025
10.22235/cp.v19i2.4332
Original Articles
Vulnerability on the Streets: A study on the Use of Psychoactive Substances among Homeless Populations
Vulnerabilidad en las calles: un estudio sobre el uso de sustancias psicoactivas en personas en situación de calle
Vulnerabilidade nas ruas: um estudo sobre o uso de substâncias psicoativas entre moradores de rua
Jorge Emilio Salazar Flórez1, ORCID 0000-0002-7666-9099
Daniella Quintero Pinzón2, ORCID 0000-0002-1983-4924
Luz América Penagos Jaramillo3, ORCID 0009-0004-7004-1964
Luz Stella Giraldo Cardona4, ORCID 0000-0003-0192-2798
1 Fundación Universitaria San Martín, Colombia, [email protected]
2 Fundación Universitaria San Martín, Colombia
3 Corporación de Profesionales Asesores, Colombia
4 Fundación Universitaria San Martín, Colombia
Abstract:
Introduction: The use of psychoactive substances in homeless individuals prolongs their time on the streets and increases the risk of acquiring chronic and infectious diseases. Objective: To identify substances use profiles in homeless individuals. Method: A cross-sectional study was conducted with 368 homeless individuals who attended the Centro Día Program in Itagüí, Antioquia, Colombia. Information related to psychoactive substance use was extracted from clinical records, with prior approval for its use. Profiles of stimulants, depressant, and hallucinogenic or psychoactive substance use affecting the Central Nervous System were created. Prevalence, prevalence ratios, and a multiple correspondence analysis were estimated. Results: A total of 88.3 % of participants were men, with an average age of 41.1 years (SD = 14.8). The prevalence of substance use was identified as 73.9 %, with hallucinogenic or psychoactive (marijuana) and depressants (alcohol) being the most common. The profile analysis showed that single men who had been on the streets for more than 3 months were more likely to consume stimulant and depressant drugs. Conclusions: The persistence of psychoactive substance use, as well as inadequate addiction management, increases social vulnerability, which can exacerbate issues such as begging and criminal behavior.
Keywords: homeless people; drug users; substance-related disorders; central nervous system stimulants; central nervous system depressants.
Resumen:
Introducción: El consumo de sustancias psicoactivas en personas sin hogar prolonga la situación de calle y aumenta el riesgo de adquirir enfermedades crónicas e infecciosas. Objetivo: Identificar perfiles de consumo de sustancias en personas en situación de calle. Método: Estudio transversal con 368 personas en situación de calle que asistieron al Programa Centro Día en Itagüí, Antioquia, Colombia. La información relacionada con el consumo de sustancias psicoactivas se extrajo de las historias clínicas previo aval para su uso. Se conformaron perfiles de consumo de sustancias psicoactivas estimulantes, depresoras e hipnóticas del sistema nervioso central. Se estimaron prevalencia, razones de prevalencia y un análisis de correspondencias múltiple. Resultados: Participaron 88.3 % varones, con una edad media de 41.1 años (DE = 14.8). Se identificó una prevalencia de consumo de sustancias del 73.9 %, con mayor frecuencia de hipnóticos (marihuana) y depresores (alcohol). El análisis de los perfiles mostró que los hombres solteros con más de 3 meses en la calle eran más propensos a consumir drogas estimulantes y depresoras. Conclusiones: La persistencia en el consumo de sustancias psicoactivas, así como la falta de un manejo adecuado de las adicciones, incrementa la vulnerabilidad social, lo que puede agravar problemas como la mendicidad y la delincuencia.
Palabras clave: población de calle; consumidores de drogas; trastornos relacionados con sustancias; estimulantes del sistema nervioso central; depresores del sistema nervioso central.
Resumo:
Introdução: O consumo de substâncias psicoativas por pessoas sem moradia prolonga a situação de rua e aumenta o risco de contrair doenças crônicas e infecciosas. Objetivo: Identificar perfis de consumo de substâncias em pessoas em situação de rua. Método: Foi realizado um estudo transversal com 368 pessoas em situação de rua que participaram do Programa Centro Dia em Itagüí, Antioquia, Colômbia. As informações relacionadas ao consumo de substâncias psicoativas foram extraídas dos prontuários clínicos, com aprovação prévia para seu uso. Foram formados perfis de consumo de substâncias psicoativas estimulantes, depressoras e hipnóticas do Sistema Nervoso Central. Foram estimadas prevalência, razões de prevalência e realizada uma análise de correspondência múltipla. Resultados: Participaram 88,3 % homens, com uma idade média de 41,1 anos (DP = 14,8). Identificou-se uma prevalência de consumo de substâncias de 73,9 %, com maior frequência de hipnóticas (maconha) e depressores (álcool). A análise dos perfis mostrou que homens solteiros com mais de 3 meses nas ruas eram mais propensos a consumir drogas estimulantes e depressores. Conclusões: A persistência no consumo de substâncias psicoativas, bem como a falta de um manejo adequado das dependências, aumenta a vulnerabilidade social, o que pode agravar problemas como a mendicância e a delinquência.
Palavras-chave: pessoas em situação de rua; usuários de drogas; transtornos relacionados ao uso de substâncias; estimulantes do sistema nervoso central; depressores do sistema nervoso central.
Received: 29/10/2024
Accepted: 19/05/2025
In Colombia, unhoused individuals are those who reside on the streets, either permanently or temporarily (Congreso de Colombia, 2013; República de Colombia & Ministerio de Salud y Protección Social, 2022). It is estimated that 154 million people, nearly 2 % of the global population, are homeless (Acuto, 2019). According to the 2019 census data from the National Administrative Department of Statistics (Departamento Administrativo Nacional de Estadística [DANE], 2021), Antioquia had 3,788 unhoused individuals, or 0.6 per 1,000 inhabitants. Most of this population was predominantly male between the ages of 25 and 39 (DANE, 2021; República de Colombia & Ministerio de Salud y Protección Social, 2022). Similarly, the 2021 national census recorded 6,248 unhoused individuals across Colombia, revealing that the primary causes of homelessness were substance abuse (33.5 %), family conflicts or difficulties (25.7 %), and economic problems (15.4 %) (DANE, 2021).
Homelessness represents an extreme manifestation of social exclusion, in which multiple forms of structural vulnerability converge, including poverty, discrimination, family violence, and substance use disorders. Understanding psychoactive substance use in this population requires not only a clinical approach, but also an analysis of the contextual dynamics that perpetuate this condition. From Bronfenbrenner’s ecological model (Bronfenbrenner & Evans, 2000), human behavior is understood as the result of interactions between the individual and multiple environmental systems (microsystem, mesosystem, exosystem, and macrosystem), which is particularly useful in interpreting substance use among homeless individuals as an adaptive response to highly adverse environments, where support networks have been broken and opportunities for social reintegration are scarce. Ecological models help identify how individual factors (such as trauma history or mental health), interpersonal factors (such as broken family ties or domestic violence), and institutional factors (such as lack of access to healthcare, employment, and housing) interact to sustain substance use and hinder recovery processes (Betancourt et al., 2023; Coleman et al., 2022; Schlarb et al., 2025).
A systematic review reported high levels of substance use among homeless children. Among the 50 studies included, 34 % were conducted in Africa, followed by South and Central America with 28 %, and Asia with 24 %. The pooled prevalence of inhalant use across these studies was 47 % (Embleton et al., 2013). The coexistence of homelessness and psychoactive substance abuse is common, acting as a reciprocal risk factor. In Colombia, 34 % of unhoused individuals remain in their situation due to substance use (DANE, 2021). In the literature, the use of hallucinogenic or psychoactive substances (e.g., cannabis) and stimulants (e.g., cocaine, cigarettes) is reported to be more prevalent (Armoon et al., 2023). These people face numerous vulnerabilities that can perpetuate substance use, such as unemployment or informal work, difficulty accessing healthcare, and multiple health issues like HIV, hepatitis, and tuberculosis, and they encounter challenging social situations with little family or social support (Bedoya-Mejia et al., 2023; Berbesi-Fernandez et al., 2014; Calderón et al., 2018). Furthermore, this population often does not utilize health or government services for re-socialization. In Medellín, a neighboring city of Itagüí, 5.3 % of unhoused individuals avoided health centers for fear of arrest, and 9.0% avoided them due to poor treatment by health personnel because of their substance use (Berbesi-Fernandez et al., 2014).
Prolonged exposure to these conditions can lead to dependence on psychoactive substances, which in turn causes changes to both their physical and mental health (Hammersley, 1996; Kemp et al., 2006). The prevalence of mental disorders, alcohol abuse, and other drug use adds to breaking with their social networks and protective groups, increasing their vulnerability (Borysow et al., 2017). Consequently, the impact on the individual is significant, but the social cost is even greater. Regarding the physical effects of substance use, intoxication is common, and in some cases, it can lead to mortality (Gaber et al., 2024). A previous study reported that up to 3.3 % of unhoused individuals might experience intoxication due to psychoactive substance use (Baron, 2018). This figure is higher in other countries. For example, in England, 17.9 % of all emergency department presentations by people experiencing homelessness were for poisoning (including drug overdose), with psychoactive substance use accounting for 12.7 % of all admissions in 2018/2019 (Paudyal et al., 2023).
Additionally, substance use reinforces aggressive behaviors, with physical aggression progressively increasing as substance consumption rises (Vegas et al., 2024). Another consequence is the increase in criminal acts; 52% of unhoused persons in Bogota were found to have committed criminal acts under the influence of psychoactive substances (Gómez et al., 2017). Consequently, interventions that encourage reduced consumption, safe use, or complete cessation benefit the individual and their family and social environment. Drug use tends to increase with age, whereas tobacco use declines as individuals get older. Risk factors associated with psychoactive substance use include being male, experiencing homelessness, having deceased parents, a family or friend history of substance use, exposure to violence, having casual sex partners, a history of working in the sex trade and engaging in unprotected sex (Armoon et al., 2023; Pares-Bayerri et al., 2023).
In Colombia, there is a context that could support the implementation of strategies to improve the situation of the unhoused population. The Decree 1285 of 2022 establishes public policy for unhoused individuals from 2022 to 2031(República de Colombia & Ministerio de Salud y Protección Social, 2022). Within this context, and recognizing previous advances made by Centro Día Itagüí (CiudadSur, 2018), it is pertinent to identify the prevalence of substance use and profiles based on its effects on the central nervous system and related situations. This information can facilitate policy implementation and the differential approach that could benefit the socialization processes and integration into social life for people experiencing homelessness. In Colombia, the challenge is greater due to the constant discrimination against substance users, with studies often reporting the prevalence of discrimination close to 62 % (Bedoya-Mejia et al., 2023). This approach allows for developing new intervention strategies based on a better understanding of their needs, health conditions, and psychosocial and socioeconomic aspects. Consequently, this study aimed to identify substance use prevalence and profiles among people experiencing homelessness from Centro Día Itagüí between 2018 and 2022.
Materials and Method
Study Design and Participants
A cross-sectional observational, descriptive study (Ato et al., 2013) was conducted with the participation of unhoused persons who are users of the Centro Día program in the municipality of Itagüí. This institution reported a census of 723 users who accessed the program between 2018 and 2022. However, after the inclusion criteria were verified, the final sample consisted of 368 records. As a criterion, information on whether they consumed psychoactive substances was required. Additionally, they had to report the specific substances used and the frequency and duration of use. Sampling was not applied. All records that met the criteria for complete data on psychoactive substance use variables were analyzed.
Instruments and variables
We had access to the users' admission form, the medical and psychological medical records, and the interventions carried out by the social work staff to collect the information on psychoactive substance use required for this research.
The participants were analyzed based on demographics (sex, age, level of education, marital status, and occupation), homelessness events (time on the street, triggering event, support network), and psychoactive substance use. The psychoactive substances used by the participants were classified according to their effects on the Central Nervous System (CNS), following their predominant pharmacological actions. Stimulants included cigarettes, cocaine, cocaine hydrochloride, and cocaine base paste, due to their excitatory effects on neurotransmitter release. Depressants include alcohol, inhalants, and benzodiazepines, which are known to suppress CNS activity and promote relaxation or sedation. Marijuana was categorized as a psychoactive substance with sedative and hallucinogenic effects, given its interaction with cannabinoid receptors (CB1 and CB2) in the CNS, which can induce states of drowsiness, altered perception, and cognitive impairment, as supported by previous neuropharmacological literature (Costardi et al., 2015; Rivera-Olmos & Parra-Bernal, 2016). Variables related to substance use included the type of substance, duration, and frequency of use, as well as previous family history of substance use and substance abuse treatment.
Procedure
Information was collected on aspects of such consumption, such as motives, type, time, and frequency. Sociodemographic and family variables were also obtained. The source of information is secondary, corresponding to medical records maintained by the Centro Día care center. The records were anonymized with a unique alphanumeric code. The data collected was entered into a pre-established matrix in Microsoft Excel software. Two researchers performed the extraction independently. To ensure better control of data extraction, two authors performed the process in parallel, allowing for the identification and correction of typing errors through weekly comparisons. On a weekly basis, the principal investigator supervised a random sample of 10 % of the total histories extracted during the week to ensure the quality of the records.
Data analysis
The information was analyzed using Stata v14.0 software. The data was analyzed using descriptive statistics such as absolute and relative frequencies for categorical variables and measures of central tendency and dispersion for quantitative variables. The prevalence of psychoactive substance use was identified. A bivariate analysis was carried out through Chi-square or Fisher's Exact Test, and the Prevalence Ratio (PR) was calculated to determine the possible variables associated with substance use according to its effects on the CNS. Finally, profiles were constructed according to the type of psychoactive substances, such as stimulants, depressants, and hallucinogenic, as the dependent variable in a Multiple Correspondence Model (MCM) with variables such as sex, age, marital status, and time on the street as independent variables. MCM was used to identify patient profiles, focusing on distinguishing between types of psychoactive substances, such as stimulants and depressants. MCM effectively reduces the dimensionality of nominal categorical data and positions this data in a factorial space using the chi-squared distance to outline relationships between categories. A 2D scatter plot illustrating the first two principal components was used for visual interpretation, grouping similar profiles and distinguishing between the three types of consumption.
Ethical considerations
This study was approved by the Ethics Committee of the Fundación Universitaria San Martín (Act No. 3 of 2022) and was classified as minimal-risk research under Resolution 8430 of 1993 from the Colombian Ministry of Health (Ministerio de Salud, 1993), as it relied on secondary data from clinical records without direct interaction with participants. All data were anonymized using alphanumeric codes, and no personally identifiable information was collected. Therefore, informed consent was not required, in accordance with national ethical guidelines and the principles of the Declaration of Helsinki (Asociación Médica Mundial, 2019). The results were socialized with the Day Center, participants, and decision-makers in the city.
Results
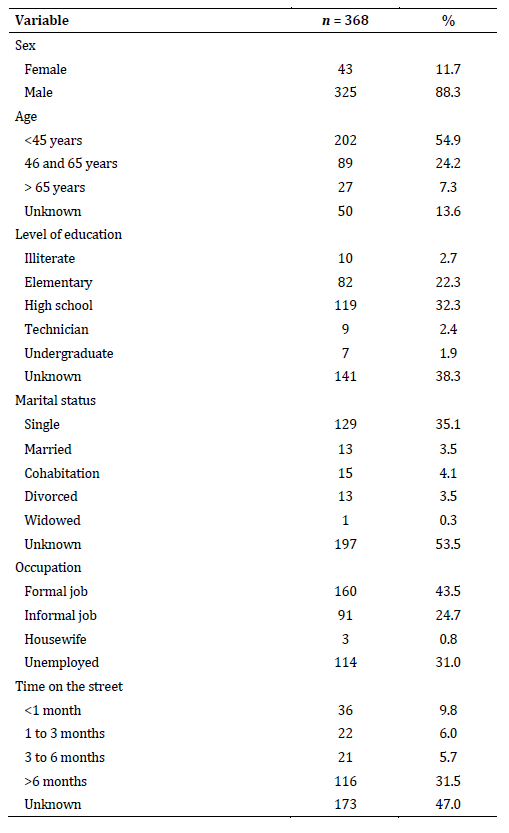
From the census that identified 723 users of the program between 2018 and 2022, 368 unhoused persons were selected who complied with the characteristic of completeness of information about the consumption of psychoactive, of whom 88.3 % were men, with ages between 16 and 80, and an average of 41.1 years (SD =14.8). Of the users, 54.6 % had an elementary or high school degree, and 38.3% did not provide this information. Regarding marital status, 35.1 % indicated that they were single, followed by cohabitation; it should be noted that 53.5 % of the users did not have this information recorded. It was found that 31.5 % of those aware of their time on the streets had been homeless for more than 6 months. Eighty-seven participants (23.6 %) identified using psychoactive substances as the trigger for their situation on the street. Only 10.6 % of the users indicated having a support network, which could be family or close friends (Table 1).
Table 1: Sociodemographic characteristics of Itagüi Centro Dia users. 2018-2022
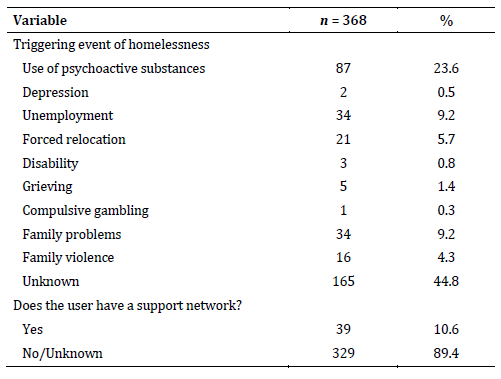
It was identified that 73.9 % (n = 272) of unhoused people consumed psychoactive substances. A total of 6.3 % (17/272) of the users reported having a close family member with a psychoactive substance use disorder, with the father figure having the highest prevalence. Table 2 shows marijuana (61.4 %), alcohol (55.1 %), cigarettes (41.5 %), and cocaine hydrochloride (41.2 %) as the substances with the highest prevalence of use. Users also reported experimental use of substances such as 2CB, amphetamines, and scopolamine, with a low proportion of participants with opioid use (1.4 %). Regarding the use time, it is observed that for all psychoactive substances, except for inhalants, use is greater than 10 years; however, it is essential to note that many users were unaware of how long they had been using (Table 2).
Table 2: Use of psychoactive substances, Itagüi Centro Dia users. 2018-2022
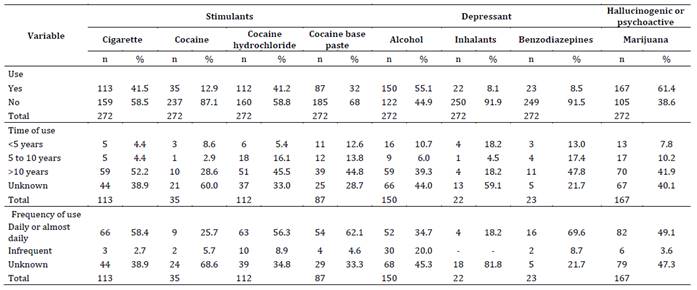
When analyzing the potential triggers of psychoactive substance use, age (p < .001) and a family history of psychoactive substance use (p = .014) were identified as associated factors. A higher prevalence of consumption was observed in younger age groups under 45 years (88.6 %), with 1.3 times the prevalence reported in those over 65 (63.0 %) and 95.7 % of individuals with a family history of substance use (Table 3).
Table 3: Possible triggers for psychoactive substance use, Itagüi Centro Dia users. 2018-2022
Note: a: Chi-square test of association. b: Fisher test.
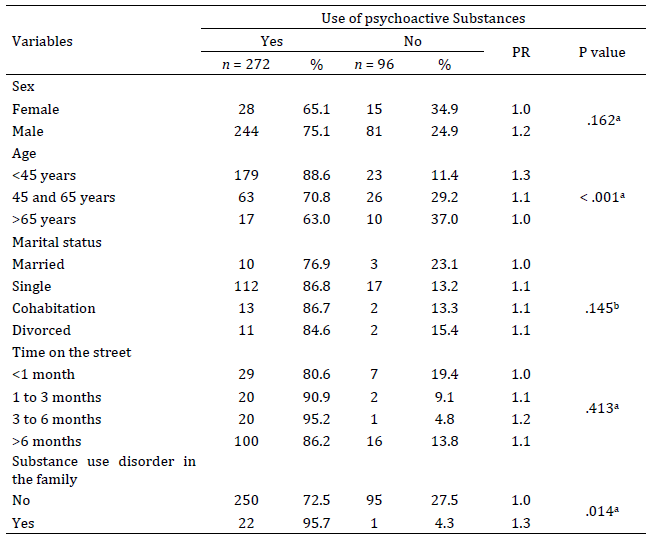
When classifying psychoactive substances according to their effects on the CNS, a higher prevalence of stimulant and hallucinogenic substance use was observed among men compared to women (RP > 1.0). Additionally, individuals under 65 years of age exhibited a higher prevalence of using all three substance groups compared to those over 65 years (RP > 1.0, p = .011). The same trend was noted among those who were single, cohabiting, or divorced, in contrast to those who were married; the former groups had higher prevalence of use for all three types of psychoactive substances (Table 4).
Conversely, having any level of education (primary, secondary, or technical) appeared to protect against the use of stimulant and depressant substances. Findings indicated a lower prevalence among educated participants than those without schooling. Participants who had been homeless for more than a month showed prevalence exceeding 80 % for stimulant use, higher than those reported for individuals who had been homeless for less than a month (RP > 1.0). Hallucinogenic or psychoactive substance use was also more prevalent among those who had been homeless for more than a month. Finally, among those who had undergone substance abuse treatment, prevalence for depressant and hallucinogenic or psychoactive substance use were below 60 %, lower than those reported among individuals who had not received treatment (Table 4).
Table 4: Associated factors with psychoactive substance use, Itagüi Centro Dia users. 2018-2022
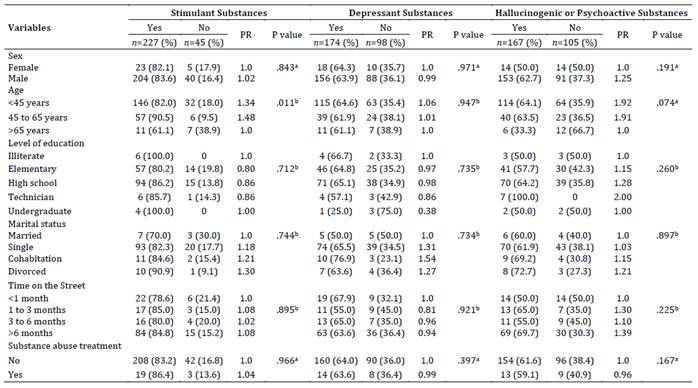
Note: a: Chi-square test of association. b: Fisher test.
Figure 1: Profile for psychoactive substance use by Multiple Correspondence Model
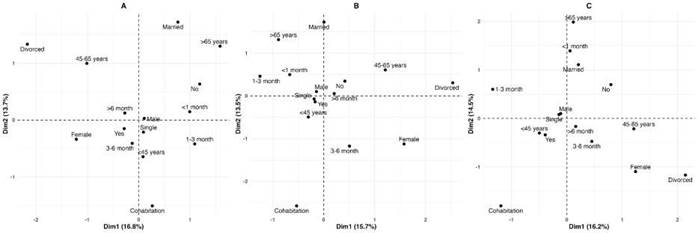
Note: Panel A: Stimulant substances. Panel B: Depressant substances. Panel C: hallucinogenic or psychoactive substances.
The multiple correspondence analysis (MCA) revealed distinct sociodemographic clustering patterns based on the type of psychoactive substance consumed. In Plot A (stimulants), the first two dimensions explained 30.5 % of the total variance (Dim 1 = 16.8%, Dim 2 = 13.7 %). Individuals who were male, single, and under 45 years old clustered near the center of the graph, along with those who had been homeless for more than six months—suggesting a persistent pattern of stimulant use during a functionally active stage of life.
In Plot B (depressants), the axes accounted for 29.2 % of the variance (Dim 1 = 15.7 %, Dim 2 = 13.5 %). Here, individuals over 65 years old and those who were married tended to group in the upper-left quadrant, while women and divorced participants appeared on the far right. This pattern may reflect gender- and age-related consumption behaviors, possibly linked to emotional decline or chronic isolation.
In Plot C (substances with sedative or hallucinogenic or psychoactive effects), the dimensions explained 30.7 % of the total variance (Dim 1 = 16.2 %, Dim 2 = 14.5 %). Although categories were more dispersed, a noticeable proximity was found among younger males (< 45 years), single individuals, and recent consumers (< 1 month), suggesting a less stable or more recent pattern of substance use. Conversely, women, divorced individuals, and those in cohabitation clustered in the lower-right quadrant, indicating alternative configurations of sedative use. These patterns help identify socio-demographic combinations of risk that can inform tailored harm-reduction strategies and psychosocial interventions for homeless populations. (Figure 1).
Discussion
This study confirmed that unhoused persons in Itagüi have a high prevalence of psychoactive substance use (73.9 %), with particularly high rates for hallucinogenic or psychoactive substances like marijuana (61.4 %), alcohol (55.1 %), which are depressants, and cigarettes (41.5 %), which are stimulants. Age and substance use in the family were usually associated with a higher prevalence of consumption (p < .05). Age, marital status, and time on the street increased the prevalence of stimulant and depressant use in the CNS, although only age showed a statistically significant relationship. Finally, no variables were associated statistically with the prevalence of hallucinogenic or depressant substance use.
A significant proportion of homelessness was attributed to the consumption of psychoactive substances (23.6 %), a finding consistent with previous studies conducted among unhoused populations in Cali (35 %) (Hernández-Carrillo et al., 2015) and Medellín (ranging from 26 % to 37 %) (Arias & Pamplona, 2015; Correa-Arango & Zapata-Posada, 2007); as well as in international context (Embleton et al., 2013). According to testimonies of unhoused persons in Bogotá, this could be explained by a greater consumption of psychoactive substances in the street environment and greater tolerance to their sale, which is why they decide to leave their homes (Alfonso et al., 2019). This reinforces that consuming psychoactive substances means deteriorating social ties, leading to a complete rupture (Farigua et al., 2018).
The results revealed a high prevalence of psychoactive substance use among individuals experiencing homelessness who participated in the Centro Día program, particularly marijuana (61.4 %) and alcohol (55.1 %). These findings are consistent with studies conducted in other urban contexts in Latin America and the United States, where these substances are commonly reported among homeless populations (Fuster & Gelberg, 2019; Hernández-Carrillo et al., 2015). Beyond availability and low cost, this pattern of use can be understood as a functional and emotional coping mechanism in response to extreme conditions such as hunger, exposure to the elements, insecurity, and social isolation. In this context, substance use reflects not only a clinical issue but also a form of psychosocial adaptation to persistent exclusion, as noted by Alfonso et al. (2019) and Motta-Ochoa et al. (2023).
In the context of life on the streets, the consumption of psychoactive substances is perpetuated as a mechanism to cope with hunger and pain, generating a mechanism of deception to the CNS to achieve greater tolerance of adverse conditions (Alfonso et al., 2019). Another of the most frequent triggers of the street situation was the problems and conflicts in the family, also reported in a study on unhoused persons in Nicaragua (Vazquez & Berrios, 2022). These situations are more marked in children and adolescents in street situations, where up to 75 % of consumption has been reported (Brasesco, 2011). In addition, it was identified that this situation could determine the length of time spent on the street, according to a finding in a Scottish study (Kemp et al., 2006), where it was established that people have an entry into the street habitat determined by family problems, the loss of children, and deterioration in general health. Still, their return home was conditioned by the absence of family problems. This evidence a complex framework of elements from the perspective of the ecological model (Bronfenbrenner & Evans, 2000), which interrelate (personal, family, community), generating the conditions for developing and/or perpetuating consumption.
Additionally, the association between younger age (< 45 years) and higher stimulant use may be linked to life trajectories marked by early exposure to high-risk environments, family disruption, and the need to remain alert in order to survive on the streets. In contrast, higher use of depressants among older adults may be related to physical decline, untreated chronic illness, or depressive states linked to social disconnection. These differences in consumption profiles by age group and substance type suggest that patterns of use are deeply shaped by structural and contextual factors, including lack of access to healthcare, limited availability of tailored treatment programs, and insufficient pathways for social reintegration (Gómez et al., 2017; Kemp et al., 2006). These findings reinforce the need for integrated, intersectoral approaches that combine public health, social inclusion, and human rights in the response to homelessness.
Regarding the type of psychoactive substances, users of the Centro Día program reported a higher use of marijuana (61.4 %), as has been observed in street inhabitants in Cali (51.2 %) (Hernández-Carrillo et al., 2015) and Los Angeles, California in the United States (78 %) (Fuster & Gelberg, 2019). Marijuana has a psychologically stimulating effect, and its biochemical and molecular components interact with the CB1 and CB2 receptors (endocannabinoid system) in various structures of the central nervous system (CNS) and immune cells. Although users of this substance seek effects of euphoria, distortion of reality, and a psychedelic experience, chronic use can cause sleep disturbances, cognitive dysfunction, anxiety, depression, and even cerebrovascular events (Rivera-Olmos & Parra-Bernal, 2016).
The next most frequently used psychoactive substance was alcohol, as shown in other studies (Almaguer & González, 2014; Usdan et al., 2001; Vazquez et al., 2020). On the contrary, a 2023 systematic review indicated that the most reported lifetime and current psychoactive substance was the stimulant tobacco, followed by cannabis, LSD/ecstasy, and cocaine (Armoon et al., 2023). Alcohol is a psychotropic depressant that affects the CNS by altering multiple neural pathways at once. The diverse effects of alcohol on the CNS lead to overall psychomotor depression, challenges in memory retention and logical reasoning, and motor coordination issues. Additionally, alcohol stimulates the reward system, which may contribute to the development of addiction (Costardi et al., 2015). As reported by homeless people in other studies use alcohol to cope with painful memories, deal with harsh living conditions, socialize/seek a sense of belonging, enjoying themselves/have fun (Motta-Ochoa et al., 2023).
In present research, it was a low proportion of unhoused persons with opioid use (1.4 %), an event that is studied mainly in industrialized countries such as the United States due to the opioid epidemic, finding prevalence rates of up to 12.5 % (Doran et al., 2018). This fact suggests that difficulties in accessing these substances do not significantly impact their consumption, given that opioids can be obtained through a medical prescription (Cardoso-Ortiz et al., 2020). Just as the consumption of psychoactive substances becomes one of the leading causes of homelessness, it is also found that unhoused persons report that they are not able to overcome their situation because they are deeply immersed in consumption and addiction (Arias & Pamplona, 2015), which leads them to resort to different methods to preserve the purchase of substances, such as begging (10 %), street vending (23 %), recycling (37 %) (Arias & Pamplona, 2015) and theft or legal problems (Hall et al., 2024; Song et al., 2021). This study identified that 24.7 % of users engaged in informal work involving street vending and recycling previous homelessness; despite this, the instrument did not ask about illegal acts.
In this study, age was significantly associated with the prevalence of psychoactive substance use, particularly stimulants. A family history of substance use was also a key factor. Previous research has indicated that among children and adolescents, the use of psychoactive substances and injectable drugs is high. However, tobacco use decreases with age, the use of injectable drugs and cocaine increases as age progresses (Armoon et al., 2023). Often, street-involved children and youth who were male, homeless, had parents who had died, had a history of substance use among family members or best friends, had experienced violence, had casual sex partners, had a history of working in the sex trade, and had unprotected sex were all related to psychoactive substance use and injecting drug use (Armoon et al., 2023). The consumption of substances showed worse indicators of effects regarding alcohol, medical and psychiatric problems, employment and family support subscales, as well as greater involvement with legal problems, violence, sexual abuse, suicide risk, and health-related problems such as HIV/AIDS, hepatitis, and tuberculosis (Halpern et al., 2017).
Taking this into account, the management of addictions in unhoused people becomes one of the keys to being able to carry out proper reintegration into society for these people, not only involving the participation of professional experts in the consumption of psychoactive but requiring the participation of the user of the program, thereby avoiding leaving the responsibility of their recovery on third parties. For this reason, the work of institutions such as Centro Día becomes a pillar when formulating strategies to address the problems related to unhoused persons. This was also observed in a meta-analysis that evaluated the effect of shelters for homeless people on aspects such as the health and well-being of adults, where a reduction in alcohol consumption was found with long-term attendance at the shelters, and a 2.5-fold improvement in household stability in people who attend shelters for a period of 18 to 24 months compared to those who have usual housing management but in conditions of abstinence (Baxter et al., 2019).
Community-based interventions, alongside harm reduction strategies, have demonstrated significant positive impacts among homeless populations (Gleason-Comstock et al., 2024; Morin et al., 2025). One study involving unhoused individuals reported that 86 % engaged in harm reduction services, with favorable outcomes—nearly three-quarters (n = 39) successfully accessed healthcare services (Brown et al., 2025). Centro Día has provided alternatives to support treatment adherence and reduce health risks, although its services remain limited in scope. In Canada, a new transitional housing program yielded promising results, including reductions in substance use, improvements in mental and emotional well-being, and enhanced socio-economic conditions (Morin et al., 2025).
Despite the contributions of this study, several limitations must be acknowledged. Cross-sectional design prevents the establishment of causal relationships between psychoactive substance use and participants’ social conditions. Additionally, data were obtained from secondary clinical records, which were not designed for research purposes and exhibited a high percentage of missing information in key variables such as educational level, marital status, and duration of substance use. This issue stemmed from the use of secondary data sources, specifically clinical and institutional records that were not originally designed for research purposes and often lacked systematically documented information. Such missing data may have introduced information bias and reduced the statistical power to detect associations in some analyses. This limitation also highlights the need to strengthen data collection processes in programs serving homeless populations by incorporating relevant sociodemographic and clinical variables in a structured and standardized manner. Doing so would support both comprehensive care delivery and the development of future research with greater methodological rigor. Validated instruments or standardized diagnostic tools were not employed to confirm substance use disorders, which may limit the accuracy of prevalence estimates. Furthermore, the study focused on a single institution in one municipality, restricting the generalizability of the findings to other homeless populations who do not access institutional programs. The predominance of male participants hindered a gender-based analysis, and variables such as experienced violence or mental health conditions, which could act as potential confounders, were not explored. Lastly, the lack of longitudinal follow-up limited the ability to assess patterns of substance use over time or the impact of interventions. These limitations highlight the need for future research by employing more robust designs, validated tools, and a comprehensive approach that considers the multidimensional nature of social vulnerability in homeless populations.
One of the strengths is the fact that a first description of the consumption of psychoactive substances by the users of the Centro Día program has been made, which will allow the institution to strengthen the processes of care and the behaviors to be followed for the processes of social inclusion into society and the referral to the reduction of risk of users who wish to join the program. Further to this, inputs are provided to territorial entities to get to know the street inhabitants of the municipality better, which will allow the creation and reformulation of public policies in mental health and public health for this population. Based on the above, the findings were shared with the institutions and the population to facilitate the social appropriation of knowledge.
Conclusions
This study confirms the high prevalence and complexity of psychoactive substance use among individuals experiencing homelessness, highlighting differentiated consumption profiles based on age, sex, civil status, and length of time on the streets. Beyond identifying patterns, these findings underscore the urgent need to develop tailored psychosocial interventions that address the structural and emotional dimensions of substance use.
Interventions should move beyond clinical or punitive approaches and prioritize harm reduction, emotional regulation, trauma-informed care, and social reintegration strategies. Programs such as Centro Día may benefit from incorporating structured psychosocial support, including individual and group counseling, motivational interviewing, and peer-based support, to improve engagement and adherence. Moreover, the identified profiles suggest the importance of designing differentiated strategies: for example, younger men with long-term street exposure may benefit from community-based outreach, while older adults and women may require integrated support services that address chronic health conditions, social isolation, and histories of violence.
Overall, the results advocate for a shift toward comprehensive, human rights-based approaches that integrate health, housing, and social services, ultimately promoting dignity, autonomy, and recovery among the most marginalized populations.
References
Acuto, M. (2019). We need a science of the night. Nature, 576(7787), 339. https://doi.org/10.1038/d41586-019-03836-2
Alfonso, O., Barrera, R. A., Bernal, P. I., Camargo, D. C., & Garzón, L. C. (2019). El ciclo mortal de los habitantes de la calle en Bogotá. Teorías, olvidos, políticas y desenlaces fatales. Revista de Economía Institucional, 21(41), 99-131. https://doi.org/https://doi.org/10.18601/01245996.v21n41.05
Almaguer, B., & González, A. (2014). Problemas relacionados con el alcohol en personas con conducta deambulante de la Habana. Medisur, 12(2), 451-455. http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1727-897X2014000200014
Arias, A., & Pamplona, J. (2015). Razones de hombres jovenes habitantes de calle, entre los 20 y 50 años, para continuar viviendo en la calle [Degree dissertation]. Universidad de Antioquia. https://bibliotecadigital.udea.edu.co/bitstream/10495/14483/1/AriasAna_2015_RazonesHombresJovenes.pdf
Armoon, B., Griffiths, M. D., & Mohammadi, R. (2023). The Global Distribution and Epidemiology of Psychoactive Substance Use and Injection Drug Use Among Street-Involved Children and Youth: A Meta-Analysis. Substance Use & Misuse, 58(6), 746-764. https://doi.org/10.1080/10826084.2023.2181036
Asociación Médica Mundial. (2019). Declaración de Helsinki de la AMM-Principios éticos para las investigaciones médicas en seres humanos. 64ª Asamblea General. Fortaleza, Brasil.
Ato, M., López, J., & Benavente, A. (2013). Un sistema de clasificación de los diseños de investigación en psicología. Anales de Psicología, 29(3), 1038-1059. https://doi.org/https://doi.org/10.6018/analesps.29.3.178511
Baron, Y. (2018). Condiciones de vida y salud de habitantes de calle en Bogotá D.C, año 2017 [Master's dissertation]. Universidad Santo Tomás. https://repository.usta.edu.co/bitstream/handle/11634/15274/2019yurybaron.pdf?sequence=8&isAllowed=y
Baxter, A. J., Tweed, E. J., Katikireddi, S. V., & Thomson, H. (2019). Effects of Housing First approaches on health and well-being of adults who are homeless or at risk of homelessness: systematic review and meta-analysis of randomised controlled trials. Journal of Epidemiology and Community Health, 73(5), 379-387. https://doi.org/10.1136/jech-2018-210981
Bedoya-Mejia, S., Ramos-Jaraba, S., & Berbesí-Fernández, D. (2023). Factores asociados a la discriminación en personas que se inyectan drogas de dos ciudades de Colombia. Health and Additions, 23(2), 10-25. https://doi.org/https://doi.org/10.21134/haaj.v23i2.865
Berbesi-Fernandez, D., Agudelo, L., Castaño, C., Galeano, P., Segura-Cardona, A., & Montoya-Velez, L. (2014). Utilización de los servicios de salud en la población habitante de calle. CES Salud Pública, 5(2), 147-153. https://doi.org/https://revistas.ces.edu.co/index.php/ces_salud_publica/article/view/3076
Betancourt, C. A., Goldberg, D. G., Hawks, B. A., & Kitsantas, P. (2023). Perspectives of homeless veterans living with substance use disorders (SUD) and mental illness. Heliyon, 9(10), e20364. https://doi.org/10.1016/j.heliyon.2023.e20364
Borysow, I. D., Conill, E. M., & Furtado, J. P. (2017). Atencao a saude de pessoas em situacao de rua: estudo comparado de unidades moveis em Portugal, Estados Unidos e Brasil. Ciência & Saúde Coletiva, 22(3), 879-890. https://doi.org/10.1590/1413-81232017223.25822016
Brasesco, M. (2011). Niños de la Calle: Buenos Aires SXXI. Ciencias Psicológicas, 1, 7-18.
Bronfenbrenner, U., & Evans, G. (2000). Developmental science in the 21st century: Emerging questions, throretical, models, research designs and empirical findings. Social Development, 9(1), 115-125.
Brown, L., Rishel, H., & Page, K. A. (2025). Voices of the unhoused from Santa Fe, New Mexico: A mixed methods study of health status, substance use, and community harm reduction program perspectives. Journal of Prevention & Intervention in the Community, 52(1), 73-97. https://doi.org/10.1080/10852352.2024.2352266
Calderón, G., Gómez, M., Zapata, J., & Dávila, L. (2018). Factores de logro en procesos de resocialización del habitante en situación de calle y consumidor de sustancias psicoactivas en Medellín, Colombia. Health and Additions, 18(2), 143-154. https://doi.org/https://bibliotecadigital.udea.edu.co/bitstream/10495/28813/1/GomezMaricelly_2018_FactoresProcesosResocializacion.pdf
Cardoso-Ortiz, J., López-Luna, K., Cuevas-Flores, M., Florez de la Torre, J., & Covarrubias, S. (2020). Farmacología y epidemiología de Opiodes. Biocencias, 7, 955. https://doi.org/https://doi.org/10.15741/revbio.07.e955
CiudadSur. (2018). En Itagüí se abrió un Centro Día para habitantes de calle. https://ciudadsur.co/en-itagui-se-abrio-un-centro-dia-para-habitantes-de-calle/
Coleman, H. L. S., Levy-Philipp, L., Balt, E., Zuiderent-Jerak, T., Mander, H., Bunders, J., & Syurina, E. (2022). Addressing health needs of the homeless in Delhi: Standardising on the issues of Street Medicine practice. Global Public Health, 17(11), 2991-3004. https://doi.org/10.1080/17441692.2021.2023605
Congreso de Colombia. (2013). Ley 1641 de 2013: Por la cual se establecen los lineamientos para la formulación de la política pública social para habitantes de la calle y se dictan otras disposiciones.
Correa-Arango, M., & Zapata-Posada, J. (2007). La otra ciudad: los habitantes de la calle. Prospectiva. Revista de trabajo social e intervención social, 12, 181-204. https://doi.org/https://doi.org/10.25100/prts.v0i12.960
Costardi, J. V., Nampo, R. A., Silva, G. L., Ribeiro, M. A., Stella, H. J., Stella, M. B., & Malheiros, S. V. (2015). A review on alcohol: from the central action mechanism to chemical dependency. Revista da Associação Médica Brasileira, 61(4), 381-387. https://doi.org/10.1590/1806-9282.61.04.381
Departamento Administrativo Nacional de Estadística. (2021). Censo Habitantes de la Calle: información 2021.
Doran, K. M., Rahai, N., McCormack, R. P., Milian, J., Shelley, D., Rotrosen, J., & Gelberg, L. (2018). Substance use and homelessness among emergency department patients. Drug and Alcohol Dependence, 188, 328-333. https://doi.org/10.1016/j.drugalcdep.2018.04.021
Embleton, L., Mwangi, A., Vreeman, R., Ayuku, D., & Braitstein, P. (2013). The epidemiology of substance use among street children in resource-constrained settings: a systematic review and meta-analysis. Addiction, 108(10), 1722-1733. https://doi.org/10.1111/add.12252
Farigua, S., Pedraza, J., & Ruiz, R. (2018). Experiencias de habitantes de calle que asisten al programa de salud Camad Rafael Uribe en Bogotá. Revista Ciencias de la Salud, 16(3), 429-446. https://doi.org/https://doi.org/10.12804/revistas.urosario.edu.co/revsalud/a.7263
Fuster, D., & Gelberg, L. (2019). Community Screening, Identification, and Referral to Primary Care, for Hepatitis C, B, and HIV Among Homeless Persons in Los Angeles. J Community Health, 44(6), 1044-1054. https://doi.org/10.1007/s10900-019-00679-w
Gaber, S. N., Franck, J., Widing, H., Hallgren, J., Mattsson, E., & Westman, J. (2024). Excess mortality among people in homelessness with substance use disorders: a Swedish cohort study. J Epidemiol Community Health, 78(8), 473-478. https://doi.org/10.1136/jech-2023-220989
Gleason-Comstock, J., Bolden, C., Locke, B., Lakshmi, N., Cobty, K., Mckenney, T., Uddin, K., Bauer, S., & Xu, J. (2024). People who use drugs engagement in substance use disorder services and harm reduction: evaluation, challenges and future direction of a community-based intervention. Substance Abuse Treatment, Prevention, and Policy, 19(1), 24. https://doi.org/10.1186/s13011-024-00601-1
Gómez, A., Zuleta, H., & Zuleta, P. (2017). Habitante de calle, seguridad y adicción: Opciones jurídicas con sustento médico. In Documentos CEDE. Edición especial No. 53. Universidad de los Andes.
Hall, N., Le, L., Abimanyi-Ochom, J., Marel, C., Mills, K., Teesson, M., & Mihalopoulos, C. (2024). Estimating the societal cost of heroin dependence in an Australian population engaged in treatment or harm reduction services. Drug and Alcohol Dependence, 264, 112447. https://doi.org/10.1016/j.drugalcdep.2024.112447
Halpern, S. C., Scherer, J. N., Roglio, V., Faller, S., Sordi, A., Ornell, F., Dalbosco, C., Pechansky, F., Kessler, F., & Diemen, L. V. (2017). Vulnerabilidades clinicas e sociais em usuarios de crack de acordo com a situacao de moradia: um estudo multicentrico de seis capitais brasileiras. Cadernos de Saúde Pública, 33(6), e00037517. https://doi.org/10.1590/0102-311X00037517
Hammersley, R. (1996). Drug use and other problems of residents in projects for the young, single homeless. Health and Social Care, 4(4), 193-199. https://doi.org/https://doi.org/10.1111/j.1365-2524.1996.tb00064.x
Hernández-Carrillo, M., Álvarez-Claros, K., & Osorio-Sabogal, I. (2015). Consumo autoreportado de sustancias psicoactivas ilegales en una población habitante de calle de Cali-Colombia. Revista de Salud Pública, 17(2), 217-228. https://doi.org/https://doi.org/10.15446/rsap.v17n2.30016
Kemp, P. A., Neale, J., & Robertson, M. (2006). Homelessness among problem drug users: prevalence, risk factors and trigger events. Health & Social Care in the Community, (14), 319-328. https://doi.org/10.1111/j.1365-2524.2006.00624.x
Ministerio de Salud. (1993). Resolución 8430 de 1993, "Por la cuál se establecen las normas científicas, técnicas y administrativas para la investigación en salud".
Morin, K., Aubin, N., Molke, D., Marsh, D., Jean, N., Carter, J., & Leary, T. (2025). Perspectives on a transitional housing program for people who use substances who experience homelessness and live with a mental health issue: a pilot study in an urban northern city in Canada. Substance Abuse Treatment, Prevention, and Policy, 20(1), 20. https://doi.org/10.1186/s13011-025-00649-7
Motta-Ochoa, R., Incio-Serra, N., Brulotte, A., & Flores-Aranda, J. (2023). Motives for alcohol use, risky drinking patterns and harm reduction practices among people who experience homelessness and alcohol dependence in Montreal. Harm Reduction Journal, 20(1), 22. https://doi.org/10.1186/s12954-023-00757-2
Pares-Bayerri, A., Calvo, F., Font-Mayolas, S., Panadero, S., & Vazquez, J. J. (2023). Differences in Drug Use among Persons Experiencing Homelessness According to Gender and Nationality. International Journal of Environmental Research and Public Health, 20(5), 407. https://doi.org/10.3390/ijerph20054007
Paudyal, V., Vohra, N., Price, M., Jalal, Z., & Saunders, K. (2023). Key causes and long-term trends related to emergency department and inpatient hospital admissions of homeless persons in England. International Journal of Emergency Medicine, 16(1), 48. https://doi.org/10.1186/s12245-023-00526-9
República de Colombia & Ministerio de Salud y Protección Social. (2022). Decreto 1285 de 2022: Por medio del cual se adiciona el Capítulo 8 al Título 2 de la Parte 9 del Libro 2 del Decreto 780 de 2016 relativo a la Política Pública Social para Habitantes de la Calle 2022 -2031.
Rivera-Olmos, V. M., & Parra-Bernal, M. C. (2016). Cannabis: efectos en el sistema nervioso central. Consecuencias terapeuticas, sociales y legales. Revista medica del Instituto Mexicano del Seguro Social, 54(5), 626-634. https://www.ncbi.nlm.nih.gov/pubmed/27428345
Schlarb, A. A., Blunden, S., Brand, S., Bruni, O., Corkum, P., Horne, R. S. C., Ipsiroglu, O. S., Quante, M., Spruyt, K., & Owens, J. (2025). The future of paediatric sleep medicine: a blueprint for advancing the field. Journal of Sleep Research, e14482. https://doi.org/10.1111/jsr.14482
Song, A., Wenzel, S. L., & Cho, Y. (2021). Child Abuse Victimization, Depression, and Substance Use Among Homeless Women: Application of General Strain Theory. Journal of Interpersonal Violence, 36(17-18), 8852-8873. https://doi.org/10.1177/0886260519853410
Usdan, S. L., Schumacher, J. E., Milby, J. B., Wallace, D., McNamara, C., & Michael, M. (2001). Crack cocaine, alcohol, and other drug use patterns among homeless persons with other mental disorders. he American Journal of Drug and Alcohol Abuse, 27(1), 107-120. https://doi.org/10.1081/ada-100103121
Vazquez, J. J., & Berrios, A. (2022). Unhappiness and casual attributions of homelessness among people living homeless in Leon (Nicaragua). Journal of Community Psychology, 50(1), 592-600. https://doi.org/10.1002/jcop.22636
Vazquez, J. J., Berrios, A. E., & Suarez, A. C. (2020). Health, disability, and consumption of psychoactive substances among people in a homeless situation in Leon (Nicaragua). Social Work in Health Care, 59(9-10), 694-708. https://doi.org/10.1080/00981389.2020.1835785
Vegas, M., Mateos-Agut, M., Fuente-Anuncibay, R., Pineda-Otaola, P., & Sebastián-Vega, C. (2024). Relación entre consumo de sustancias y agresividad, problemas académicos, familiares y conductuales en adolescentes españoles. Health and Additions, 12, 1-20. https://doi.org/https://doi.org/10.21134/778
Data availability: The dataset supporting the results of this study is not available.
Funding: This study was financed in part by the San Martín University Foundation, PYI-2021-009 Diagnosis of the health situation of adult street dwellers in Medellín, 2019/2021 [Diagnóstico de la situación de salud del adulto habitante de calle de Medellín, 2019 - 2021].
Conflict of interest: The authors declare that they have no conflicts of interest.
How to cite: Salazar Flórez, J. E., Quintero Pinzón, D., Penagos Jaramillo, L. A., & Giraldo Cardona, L. S. (2025). Vulnerability on the Streets: A study on the Use of Psychoactive Substances among Homeless Populations. Ciencias Psicológicas, 19(2), e-4332. https://doi.org/10.22235/cp.v19i2.4332
Authors’ contribution (CRediT Taxonomy): 1. Conceptualization; 2. Data curation; 3. Formal Analysis; 4. Funding acquisition; 5. Investigation; 6. Methodology; 7. Project administration; 8. Resources; 9. Software; 10. Supervision; 11. Validation; 12. Visualization; 13. Writing: original draft; 14. Writing: review & editing.
J. E. S. F. has contributed in 1, 3, 4, 5, 6, 7, 8, 10, 11, 14; D. Q. P. in 2, 3, 5, 12, 13, 14; L. A. P. J. in 5, 6, 11, 14; L. S. G. C. in 3, 5, 6, 9, 11, 12, 13, 14.
Scientific editor in-charge: Dr. Cecilia Cracco.
Ciencias Psicológicas; v19(2)
July-December 2025
10.22235/cp.v19i2.4332
Original Articles