10.22235/cp.v18i2.3667
Original Articles
The effectiveness of psychotherapies in reducing further suicide attempts: a systematic review with meta-analysis of randomized controlled trials
A eficácia de psicoterapias na redução de novas tentativas de suicídio: uma revisão sistemática com meta-análises de ensaios clínicos randomizados
La efectividad de las psicoterapias en la reducción de nuevos intentos de suicidio: una revisión sistemática con metanálisis de ensayos clínicos aleatorios
Luciana Almeida Santos1, ORCID 0000-0003-4151-2785
Maycoln Leôni Martins Teodoro2, ORCID 0000-0002-3021-8567
Fellipe Couto De Oliveira3, ORCID 0009-0003-6365-1417
1 Universidade Federal de Minas Gerais, Brazil, [email protected]
2 Universidade Federal de Minas Gerais, Brazil
3 Universidade Federal de Minas Gerais, Brazil
Abstract:
There is little evidence on the effectiveness of psychotherapeutic interventions in reducing new suicide attempts. This article aims to evaluate the effectiveness of psychotherapeutic interventions in reducing suicide attempts among patients with a history of previous attempts. We selected 17 articles from four databases: PubMed, Cochrane, APA PsycInfo and LILACS, in 2023. Six studies showed statistical differences that favored psychotherapeutic intervention at some point during the follow-up period. These psychotherapies addressed: problem-solving, hope induction, skills training. When comparing psychotherapy with usual care, a meta-analysis revealed an odds ratio of 0.41 (95 % CI, 0.17-0.99, p = .05) in the analysis up to 12 months of follow-up, and an odds ratio of 0.48 (95 % CI, 0.30-0.78, p < .001) after 12 months of follow-up. The results indicate the efficacy of these interventions in reducing additional suicide attempts, but they should be analyzed with caution, given the heterogeneity of the sample, treatments, and comparators. This review supports the development of prevention strategies indicated for patients who have attempted suicide.
Keywords: suicide attempt; psychotherapy; randomized clinical trial; efficiency.
Resumo:
Há poucas evidências sobre a eficácia das psicoterapias na redução de novas tentativas de suicídio. Este artigo tem como objetivo avaliar a eficácia das intervenções psicoterapêuticas na redução de tentativa de suicídio em pacientes com histórico de tentativas anteriores. Selecionamos 17 artigos de quatro bases de dados: PubMed, Cochrane, APA PsycInfo e LILACS, em 2023. Seis estudos mostraram diferenças estatísticas que favoreceram a intervenção psicoterapêutica em algum momento durante o período de acompanhamento. Essas psicoterapias abordaram: resolução de problemas, indução de esperança, treinamento de habilidades. Ao comparar a psicoterapia com o tratamento usual, uma meta-análise revelou um odds ratio geral de 0,41 (IC 95 %, 0,17 a 0,99, p = 0,05) na análise até 12 meses de acompanhamento, e um odds ratio de 0,48 (IC 95 %, 0,30 a 0,78, p < 0,001) após 12 meses de acompanhamento. Os resultados apontam para a eficácia dessas intervenções na redução de novas tentativas de suicídio, mas devem ser analisadas com cautela, dada a heterogeneidade da amostra, tratamentos e comparadores. Esta revisão oferece suporte para o desenvolvimento de estratégias de prevenção indicada para pacientes que tentaram suicídio.
Palavras-chave: tentativa de suicídio; psicoterapia; ensaio clínico randomizado; eficácia.
Resumen:
Hay poca evidencia sobre la eficacia de las psicoterapias para reducir los nuevos intentos de suicidio. Este artículo tiene como objetivo evaluar la efectividad de las intervenciones psicoterapéuticas en la reducción de los intentos de suicidio entre pacientes con intentos previos. Se seleccionaron 17 artículos de cuatro bases de datos: PubMed, Cochrane, APA PsycInfo y LILACS. Seis estudios mostraron diferencias estadísticas que favorecieron la intervención psicoterapéutica en algún momento durante el período de seguimiento. Estas psicoterapias abordaron: resolución de problemas, inducción de esperanza y entrenamiento de habilidades. Al comparar la psicoterapia con el tratamiento habitual, el metanálisis reveló un odds ratio de 0.41 (IC del 95 %, 0.17 a 0.99, p = .05) en el análisis hasta los 12 meses de seguimiento, y un odds ratio de 0.48 (IC del 95 %, 0.30 a 0.78, p < .001) después de 12 meses de seguimiento. Los resultados apuntan a la eficacia de estas intervenciones para reducir los intentos de suicidio adicionales, pero deben analizarse con cautela, dada la heterogeneidad de la muestra, los tratamientos y los comparadores. Esta revisión apoya el desarrollo de estrategias de prevención indicadas para pacientes que han intentado suicidarse.
Palabras clave: intento de suicidio; psicoterapia; ensayo clínico aleatorio; eficiencia.
Received: 07/09/2023
Accepted: 05/09/2024
Suicidal behavior (ideation, planning, attempt, and death by suicide) is a serious public health problem and is related to multiple causes. It is a complex phenomenon that can be prevented (World Health Organization (WHO), 2019). It can be understood as a continuum, in which there is a progression that begins with thoughts of death, known as suicidal ideation, followed by planning, and progressing to attempts when a person deliberately seeks a method to end their life, but their action does not result in death (Botega, 2023; WHO, 2019). Finally, death by suicide is the last stage of this process and reflects failures in all possibilities of relieving suffering and emotional pain.
There are divergences in the literature regarding the definition of suicidal behavior. Silverman (2006) defines a suicide attempt as a self-inflicted, potentially harmful behavior with a non-fatal outcome for which there is explicit or implicit evidence of intent to die. Other researchers (Almondes & Teodoro, 2020; Botega, 2023; Nock et al., 2008; Wenzel et al., 2010) define a suicide attempt when the subject deliberately seeks a method to end his own life, but his action does not result in death. In the 2014 WHO report, self-mutilation without suicidal intent is included in the definition of attempted suicide. This review defines a suicide attempt as a self-injurious act, regardless of the methods used, in which the intent to kill is clear, being distinguished from self-mutilation without the intent to kill, but we understand that this distinction is not easy: It is believed that this definition is important for implementing specific interventions and for better analysis of results.
According to the WHO (2019), suicide was the second leading cause of death among individuals aged 15 to 29 years old and the third leading cause of death among those aged 15 to 19 in 2016. For every death by suicide, there are 10 to 30 suicide attempts (Center for Disease Control and Prevention, 2016). In Brazil, according to the Mortality Information System, suicide is identified as the second leading cause of death among adolescents aged 15 to 19 years old and the fourth leading cause among young adults aged 20 to 29 years old (Brazil, 2024). A prior suicide attempt is the single greatest risk factor for further attempted or death by suicide, an outcome that generates great emotional, social, and economic impacts (Arias et al., 2016; Probert-Lindström et al., 2020; Torre-Luque et al., 2021; WHO, 2014). Preventative measures recommended for groups at high risk of further suicide attempts (Bertolote, 2012; Botega, 2023; WHO, 2014) include specific psychotherapeutic interventions, which can help the subject deal with moments of crisis, by favoring the development of psychological strategies for coping with suffering.
In recent years, some reviews have sought to systematize these findings, however, the results remain controversial. Labelle et al. (2015) performed a systematic review with a meta-analysis of 14 studies on the effectiveness of Cognitive Behavioral Therapies (CBT) for reducing suicidal behavior and self-harm in adolescents. The authors observed no significant reduction in suicide attempts. In another systematic review, the effectiveness of CBT in reducing suicidal ideation and behavior (face-to-face or online) was investigated: Leavey and Hawkins (2017) concluded that there was an effect, ranging from small to medium, in favor of face-to-face CBT in reducing suicidal ideation, attempt, and death by suicide. However, there was significant heterogeneity between the studies included. A systematic review by Jeong et al. (2023), which included 26 articles, confirmed the effectiveness of CBT in preventing new suicide attempts among individuals with a history of suicide attempts, compared to usual treatment.
The level of evidence and grade of recommendation for treating psychological disorders in children, adolescents, and adults in Spain were reviewed by Fonseca-Pedrero et al. (2021a; 2021b). For suicidal behavior in children and adolescents, these authors highlighted Dialectical Behavioral Therapy (DBT) as having a high grade of recommendation, followed by psychotherapies such as Interpersonal Psychotherapy for Adolescents, Integrated CBT, Mentalization-Based Therapy for Adolescents, the Program for Parents and Adolescents, Integrated Family Intervention, Psychoeducation, Teens Options for Change, As Safe As Possible, and Family Intervention for Suicide Prevention. Regarding the review of the level of evidence and grade of recommendation for treatments of psychological disorders in adults, Fonseca-Pedrero et al. (2021b) emphasized CBT and cognitive therapy (CT), along with DBT, especially for individuals with borderline personality disorders, and active contact and follow-up of cases, all of which have a high degree of recommendation. Next came the safety plan, brief intervention programs for individuals who have attempted suicide, and collaborative assessment and management of suicidal behavior.
Psychotherapeutic interventions are prevention methods indicated for people with previous suicide attempts, addressing feelings, thoughts, and behaviors related to the suicide attempt, problem-solving, stress management, and emotional regulation (Torre-Luque et al., 2021). Psychotherapy was defined for this study as an intervention (with or without prior theoretical guidance), in which individuals were invited to work on risk factors, protective factors, and strategies related to problem-solving for issues that triggered the suicide attempt. There was no selection of a theoretical approach, considering techniques that encompass both psychodynamic aspects and cognitive-behavioral techniques. After a suicide attempt, interventions that combine psychodynamic understanding with cognitive and behavioral approaches, that provide comprehensive, empathetic, and supportive listening are sought (Rogers, 1995). The aim is to address and alleviate what Shneidman (1993) described as unbearable psychic pain. Wenzel et al. (2010), who studied CBT for suicidal patients, stated that therapy can offer patient’s tools to modify schemas and address issues such as hopelessness, impulsivity, cognitive distortions, and problem-solving difficulties, thus helping individuals overcome dichotomous thinking. Linehan (2018) developed DBT for patients with personality disorders and suicidal behavior, which includes individual psychotherapy, group skills training, telephone coaching, and a consultation team for therapists. In psychodynamic theories, suicide is often related to traumatic content and unconscious causes of suffering; therefore, therapy aims to provide access to and reframe repetitive behaviors for better understanding. Through speech, the individual is invited to name the acts of pain that triggered the suicide attempt, potentially finding other solutions (Macedo & Werlang, 2004). According to Botega (2023), it is essential to integrate various aspects of psychological approaches for moments of crisis, such as suicide attempts.
There is little good-quality evidence regarding the effectiveness of psychotherapeutic interventions, especially from randomized clinical trials for reducing suicidal behavior (Briggs et al., 2019; Cuijpers et al., 2013, Hepp et al., 2004; Wenzel et al., 2010). Additionally, many suicide attempt reduction studies rely on contact interventions with case management, phone calls, or coping card (Malakouti et al., 2022; Messiah et al., 2019; Mousavi et al., 2016; Wang et al., 2016). Other studies investigating the effectiveness of psychotherapies did not distinguish between samples, that mixed patients with ideation, suicide attempts, and self-mutilation without suicidal intent, making it difficult to analyze the results (Briggs, 2019; Grupp-Phelan et al., 2019; Hepp et al., 2004; Ougrin et al., 2015; Rudd et al., 2015). Thus, studies scarce with good quality methodology, looking at the effectiveness of psychotherapeutic interventions to reduce suicide attempts exclusively in patients with prior attempts. As such, the objective of this systematic review with metanalysis was to evaluate the efficacy of psychotherapies in reducing further suicide attempts in adolescents, adults, and the elderly. We selected only randomized clinical trial studies that reported psychotherapeutic interventions in patients with previous suicide attempts.
This paper attempted to find articles that addressed crisis intervention from various theoretical perspectives, focusing on emerging personal and social issues to reduce suicide risk. In addition, these interventions would aim to reinforce adaptive mechanisms and healthy aspects of the personality, mitigate triggers, relieve symptoms, increase self-esteem, and strengthen protective factors.
Materials and methods
This systematic review was conducted according to the protocol previously published, Prospero (https://www.crd.york.ac.uk/prospero/#recordDetails) under Id CRD42022299424, with minor changes, as in the title. A suicide attempt was assessed by the number of repeated events and/or the number of people who repeat the suicide attempt following intervention. The number of events is related to how many new suicide attempts occurred and the number of people is related to the number of people who attempted or did not attempt suicide again over a given period.
The PICO strategy (Patient or Problem; Intervention; Control or Comparison, Outcomes) was used to construct the research question (Santos et al., 2007). The question was: “Which psychotherapies are effective for reducing suicide attempts?” which P corresponded to People with previous suicide attempts; I to Psychotherapy; C to control/comparison treatment; and O to reduction in suicide attempts. We selected randomized clinical trials of patients over eleven years of age who had previously attempted suicide, excluding patients with only suicidal ideation or self-mutilation without suicidal intent. The acronym TAU (treatment as usual) is used to refer to standard or usual treatment, appearing in studies as a comparative group, which can vary from referral to various treatment modalities to simple advice for patients seeking help.
Research Strategy
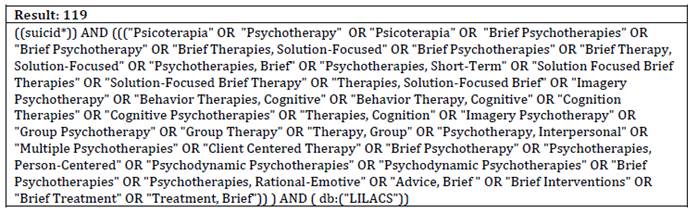
At first, a preliminary research strategy search was developed using terms from three articles that fit within the pre-defined inclusion and exclusion criteria. The strategy was validated by testing the identification of these studies. A careful search was carried out in November 2021 in the PubMed, Cochrane, LILACS, and APA PsycInfo databases. This search was repeated in February 2023. The research strategy used the descriptors MESH: suicide attempted*, psychological intervention*, randomized controlled trial*, and their synonyms. The Boolean operators 'AND', 'OR', and 'NOT' were used. A table with the detailed search strategy is available in the supplementary material. All the literature found was sent to the Rayyan application (Ouzzani et al., 2016). Next, duplicate articles were identified and excluded, followed by a blind selection of articles by title and abstract by two researchers.
The inclusion criteria were studies with a randomized clinical trial design, which investigate psychotherapies to reduce suicide attempts in populations presenting prior attempts. Interventions not classified as psychotherapy, but with similar elements were also included, as well as the surveys in which suicide attempt was a main or secondary outcome. Study participants were older than eleven years and there was no defined follow-up period and time or language filter. No selected article was presented in a language other than English.
Exclusion Criteria
Exclusion criteria were studies with specific treatments or preventative measures in school environments; single psychoeducation sessions; interventions involving only monitoring and assessment of suicide risk with visits or phone calls; interventions in which there was only one session to encourage participation, continuity of care or assessment of suicide risk; isolated interventions with cards, crisis cards, and gatekeepers. Furthermore, articles not available online or free of charge were excluded.
Meta-analysis
Meta-analysis was performed using 95 % confidence intervals (CIs), with a p-value less than .05 for statistically significant results (Rodrigues & Ziegelmann, 2010). Heterogeneity in the survey results obtained was analyzed using the I² test, considering a p-value of less than .10 as statistically significant. An I² can be low, moderate, and high to values of 25 %, 50 %, and 75 % (Higgins et al., 2003). The random effect model was applied because there are always heterogeneous aspects that are intrinsic to studies. RevMan software (Review Manager, V.5.3) was used to perform the analysis of the dichotomous outcome data, reporting the odds ratios (ORs) with a corresponding 95 % CI. A forest plot was performed showing individual information from each study, and from the final measure of the meta-analysis (Roever, 2016).
Results
Results were reported using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (Prisma) (Page et al., 2021) criteria. Data extraction was performed independently by two reviewers. The extracted data are sample characteristics, intervention details, control treatment and/or other active treatments, follow-up interval, and outcomes (the number of attempts and/or the total number of people who attempted suicide). The discrepancies between the reviewers were resolved by consensus. Data were pooled for meta-analysis in which participant, follow-up, treatment, and comparator groups were similar.
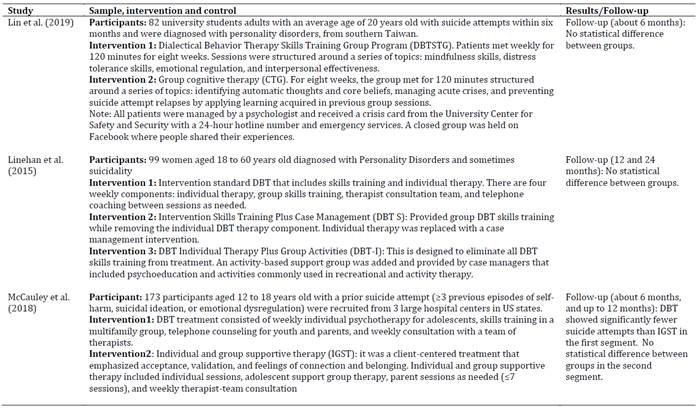
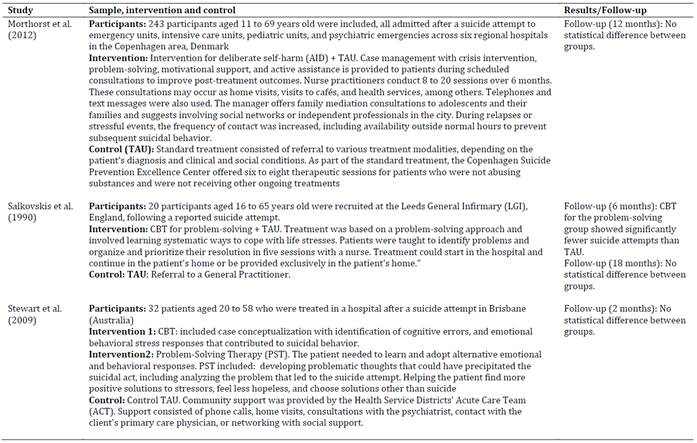
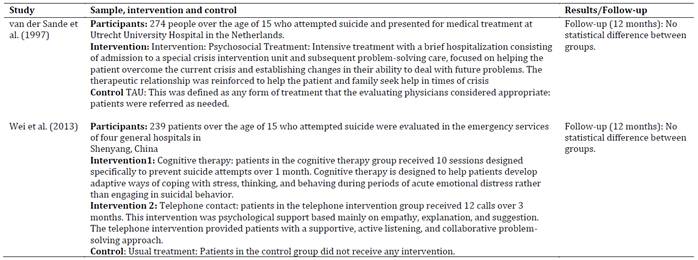
After removing duplicates, 1912 manuscripts remained, with 156 being selected for a complete reading. Through the reading of titles and abstracts, considering the inclusion and exclusion criteria described. Additionally, 18 articles found in the bibliographic references of systematic reviews with objectives similar to those of this study were included. Seven articles could not be found and were therefore discarded. After a complete reading, 17 articles remained, corresponding to 16 studies, which met this review's inclusion and exclusion criteria. Most studies were excluded because they did not limit their sample to only patients with suicide attempts. The Prisma flowchart is presented in Figure 1, and data extraction is described in Table 1.
Suicide attempts were evaluated in different ways, including self-reporting and/or through consultation of hospital records. The results presented suicide attempt measures according to the number of participants who tried again during a given period or by the number of attempts made during a given period. The time until the next suicide attempt was also measured in some articles, but not considered in this review.
Seventeen randomized clinical trials were included in the systematic review. Sample sizes ranged from 20 to 274 patients, with a total of 2068 participants (considering that one study was developed in two articles). Follow-up periods ranged from two months to five years. The number of psychotherapy sessions varied from three to 20. All interventions took place in person. There was no differentiation by gender, and the minimum age of participants was 11 years old, as reported in the study by Morthorst et al. (2012).
For comparison purposes, studies were classified as follows: psychotherapy x TAU; psychotherapy x psychotherapy (different lines of approach, or the same line with emphasis on different aspects); and psychotherapy x specific treatment (telephone contact or case management). In addition, it was not possible to establish a division by theoretical approach. Two studies used three comparators (Stewart et al., 2009; Wei et al., 2013): they were categorized according to the second comparator.
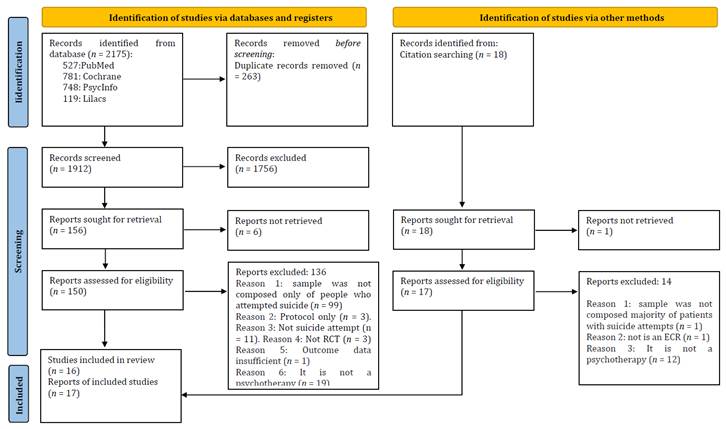
Figure 1: PRISMA
flow diagram for systematic reviews
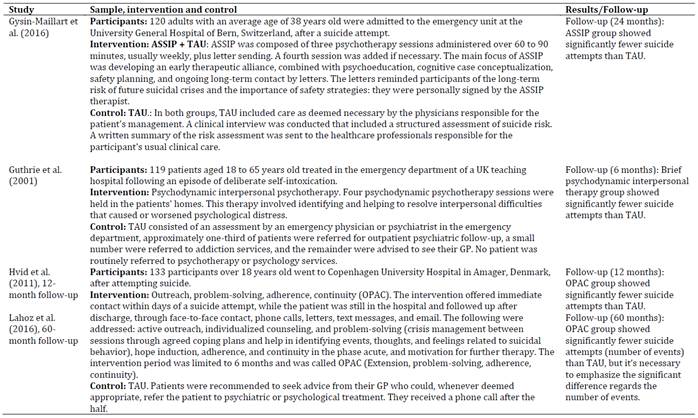
Table 1: Data extracted from the articles selected for systematic review
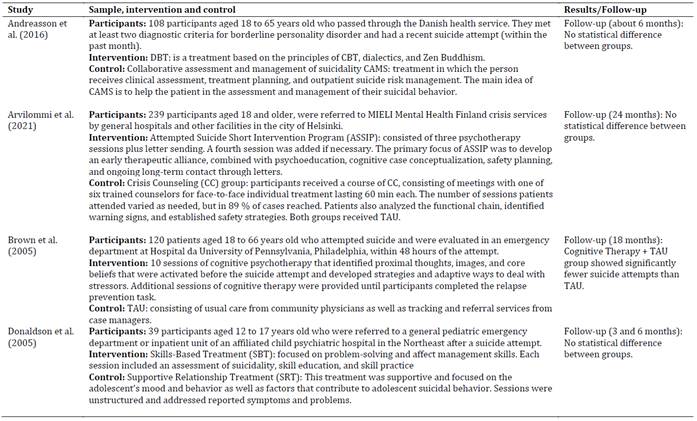
Studies comparing psychotherapeutic intervention with TAU (8 studies/ 9 articles)
The psychotherapy x TAU comparison included nine articles, two of which came from the same study (Hvid et al., 2011; Lahoz et al., 2016). Of the nine articles, five showed a statistically significant difference favoring the intervention in the number of events and/or in the number of participants with new attempts at the end of the proposed follow-up. One article (Salkovskis et al., 1990) showed a statistically significant difference favoring intervention at six months, but not at the end of the proposed 18-month follow-up period.
Interventions that showed a statistically significant difference were performed individually. The ASSIP added to the TAU (Gysin-Maillart et al., 2016) showed significant differences in the number of participants who made subsequent suicide attempts. Likewise, Brown et al. (2005) observed statistically significant differences between the number of participants and events comparing a 10-session cognitive therapy plus TAU with TAU alone. In another study, the Outreach, Problem-solving, Adherence, and Continuity (OPAC) intervention showed significant differences between events and the number of participants with new suicide attempts at 12 months and a statistically significant difference in terms of events at a 60-month follow-up (Hvid et al., 2011; Lahoz et al., 2016). The study by Guthrie et al. (2001) offered four sessions of Psychodynamic Interpersonal Therapy to patients, helping them to resolve interpersonal difficulties that caused or aggravated psychological distress. The results showed that there was a decrease in the number of patients who attempted suicide in the intervention group. The study by Salkovskis et al. (1990) investigated Cognitive Behavioural Problem Solving. The results showed a significant difference in the number of people who attempted suicide, favoring intervention at 6 months, but this difference was not observed at 18 months.
Comparative studies between psychotherapeutic interventions (6 studies)
In this comparison, DBT was investigated in three articles. In the article by Linehan et al. (2015) different DBT modalities were compared, while Lin et al. (2019) compared the effectiveness of the Dialectical Behavior Therapy Skills Training Group (DBTSTG) with the Cognitive Therapy Group (CTG). These studies did not observe differences between groups. The third study compared DBT with Individual and Group Supportive Therapy (IGST) (McCauley et al., 2018). In the latter article, DBT was statistically favorable to the comparison treatment at the six-month follow-up, but this difference did not remain after 12 months.
In addition to DBT, Stewart et al. (2009) compared CBT with Problem-Solving Therapy and with TAU. Results did not differ between the groups. Arvilommi et al. (2021) and Donaldson et al. (2005) also observed no difference. While the first compared the ASSIP program with the Crisis Counseling (CC) program, the latter investigated groups of patients undergoing Skills-Based Treatment (SBT), which focused on problem-solving and emotional management in adolescents, with the Supportive Relationship Treatment (SRT), focused on changing the mood and behavior of adolescents.
Studies comparing psychotherapeutic interventions with other interventions (2 studies)
In the study by Andreasson et al. (2016) DBT was compared with the Collaborative Assessment and Management of Suicidality (CAMS), which seeks to help patients evaluate and manage suicidal behavior. There was no statistically significant difference between the groups. In the study by Wei et al. (2013), ten sessions of Cognitive Therapy were compared with two other groups, TAU and telephone contact, which consisted of 12 calls that provided patients with support, active listening, and collaborative problem-solving. While the Cognitive Therapy and telephone intervention groups had one patient each (1.2 % and 1.3 %, respectively) make a further suicide attempt, the control group had five patients (6.5 %): there was no statistically significant difference between the groups. This study appeared to have a high dropout rate among participants.
Data analysis of the articles where there was a statistically significant difference favoring the intervention
Here are other measures reported by articles that showed significant differences between groups at some point during follow-up: in the study by Gysin-Maillart et al. (2016), the authors reported that the difference between groups in the number of participants who attempted suicide again was significant (log-rank/Mantel-Haenszel test, mean χ²₁ = 16.5, 95 % CI 15.4–17.6; mean p < .001). The mean risk ratio was 0.17 (95 % CI 0.07-0.46), indicating that the ASSIP group had an 83 % lower risk of attempting suicide during the 24-month follow-up compared to the control group (Wald χ²₁ = 13.1, 95 % CI 12.4–13.7, p < .001). Brown et al. (2005) found results indicating that participants in the cognitive therapy group (Wald χ²₁ = 3.9; p = .049; log-rank χ²₁ = 4.0; p = .045) had a significantly lower rate of reattempts compared to those in the usual treatment group (log-rank χ²₁ = 4.0; p = .045). The risk ratio for this analysis was 0.51 (95 % CI 0.26-0.997), suggesting that participants in the cognitive therapy group had a 50 % lower probability of attempting suicide during the follow-up period compared to participants in the usual treatment group. Guthrie et al. (2001) observed that at six months, five patients (9 %) in the intervention group self-harmed again, compared to 17 patients (28 %) in the usual treatment group (p = .009, Fisher’s exact test, proportion difference 19.3 %, 8.6 % to 30.0 %). Salkovskis et al. (1990) used Fisher’s exact test and found that the difference in the proportion of patients who repeated a suicide attempt within six months was significant (none in the experimental group and three patients with four attempts in the control group; p = .049). In the follow-ups by Hvid et al. (2011) and Lahoz et al. (2016), of the 69 patients in the intervention group, 6 repeated a suicide act after 1 year and 17 repeated a suicide attempt after 5 years. Of the 64 patients in the control group, 14 repeated a suicide act after 1 year and 19 repeated a suicide attempt after 5 years. Significance calculations performed by the log-rank test show that the effect on the number of patients repeating a suicide act is no longer significant at the 5 year follow-up (p = .0658). A calculation for the number needed to treat over 1 year showed benefit with 7.8 patients, indicating that eight patients had to be included in the program to prevent one patient from repeating the behavior. McCauley et al. (2018) converted the ORs to number needed to treat estimates, for the DBT group to have an additional adolescent with no suicide attempt compared with the IGST group, the number needed to treat was 8.46. Significant advantages were found for DBT on all primary outcomes after treatment: suicide attempts (65 (90.3 %) of 72 receiving DBT vs 51 [78.9 %] of 65 receiving IGST with no suicide attempts; odds ratio (OR), 0.30; 95 % CI, 0.10-0.91).
Risk of bias
An independent assessment of the risk of bias using the Cochrane RoB 2 tool was performed by two reviewers (Sterne et al., 2019). This tool includes five domains: randomization process (D1); deviations from intended interventions (D2); missing outcome data (D3); measurement of the results (D4); and selection of the reported results (D5). Results showed 3 records with a low risk of bias (Hvid et al., 2011; Lahoz et al., 2016; Morthorst et al., 2012), 12 with some concerns (Andreasson et al., 2016; Brown et al., 2005; Donaldson et al., 2005; Gysin-Maillart et al., 2016; Guthrie et al., 2001; LaCroix et al., 2018; Lin et al., 2019; Linehan et al., 2015; McCauley et al., 2018; Salkovskis et al., 1990; van der Sande et al., 1997; Wei et al., 2013), and 2 studies raised major concerns (Arvilommi et al., 2021; Stewart et al., 2009). It is important to note that no risk of bias assessment tool is completely objective. The RoB 2 tool involves interpretation and judgment by reviewers at various stages, which can introduce subjectivity.
Meta-Analysis
The results from articles that used the “intent-to-treat model” as a data analysis method were analyzed. The variable used was the number of people who attempted suicide again.
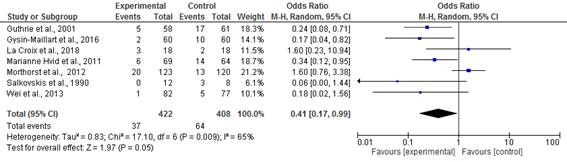
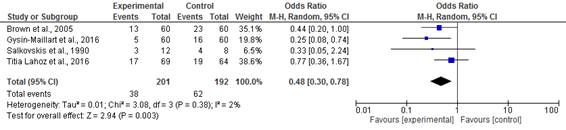
12-month Follow-up: The results using the odds ratio, the Mantel-Haenszel (MH) test, and the random effect point to a non-significant difference between the experimental group and the treatment as usual (TAU), with significant heterogeneity, considered substantial, assuming a p less than .10. This heterogeneity can be explained by the follow-up period and the diversity of participants. The study with the greatest weight, due to sample size and variability, was Morthorst et al. (2012) while the one with the least weight was Salkovskis et al. (1990). The odds ratio was 0.41 with 95 % CI, 0.17 to 0.99, p = .05, but the result was not statistically significant, with a p-value = .05 (Figure 2).
Figure 2: Effects of psychotherapeutic interventions versus TAU on the number of people who attempted suicide up to 12 months
Follow-ups beyond 12 months: The result using the odds ratio and random effect favored intervention, with a non-important and non-significant heterogeneity, considering a p less than .10. The study presenting the greatest weight was Lahoz et al. (2016) while the one with the least weight was Salkovskis et al. (1990). The odds ratio of a new suicide attempt occurring after 12 months in patients who received psychotherapy was 0.48 compared to those who received care as usual with a 95 % CI, 0.30 to 0.78, p = .0003, showing that the chance of a new suicide attempt was 52 % lower in the experimental treatment (Figure 3).
It was not possible to perform funnel chart analysis because the selected group of studies was too small.
Figure 3: Effects of psychotherapeutic interventions versus TAU on the number of people who attempted suicide after 12 months
Discussion
This systematic review sought to verify the efficacy of psychotherapeutic interventions for the reduction of suicide attempts in randomized clinical trial studies. Seventeen articles were found with samples of patients with previous attempts, from which seven (six studies) presented statistical differences that favored psychotherapeutic intervention at some point during follow-up. These interventions had a restricted number of sessions, and addressed: early therapeutic alliance, psychoeducation, safety planning, ongoing long-term contact, identifying and helping to resolve interpersonal difficulties that caused or worsened psychological distress, problem-solving, hope induction, adherence, and continuity in the phase acute, motivation for further therapy, and skills training. Although only a low percentage of articles presented this difference favoring intervention (41.17 %), no article presented a statistical difference unfavorable to intervention, leading us to conclude that these therapies require further investigation given their possible contribution to therapeutic methods for suicide prevention.
In an analysis by comparative group, the studies that most frequently presented significant results were those adopting treatment as usual as a comparator (60 %). It is notable, however, that the character of TAU is strongly dependent on the study location and presents significant differences between locations. For example, the study by Morthorst et al. (2012), carried out in Denmark, found that one of the reasons for the lack of results favorable to experimental intervention was the quality of the service provided by the Center for Excellence in Suicide Prevention in Copenhagen. On the other hand, the frequency of results in favor of intervention indicates that the local treatments available to patients can be improved. This conclusion is supported by the results from Inagaki et al. (2019), who analyzed the effect of active contact initiated in the emergency room and follow-up interventions on the risk of further suicide attempts. Results from meta-analyses suggest that active contact and follow-up interventions reduce the risk of a new suicide attempt within six months in patients admitted to an emergency department with a suicide injury. Contact interventions show promise and can be investigated as a potential complement to successful psychotherapeutic interventions as in Gysin-Maillart et al. (2016).
The follow-up time ranged from two to 60 months. Some studies showed clear results favoring intervention only over a short-term follow-up period (Lahoz et al. 2016; McCauley et al. 2018; Salkovskis et al., 1990). Other studies, such as those that worked with very small samples (Donaldson et al., 2005; LaCroix et al., 2018; Salkovskis et al., 1990; Stewart et al., 2009) or with very specific ones (Andreasson et al. 2016; LaCroix et al., 2018; Lin et al., 2019; Linehan et al., 2015; McCauley et al. 2018) may have their external validity compromised and need to be replicated with larger, more diverse samples.
Of the 17 articles found in this study, seven used Cognitive Therapy as a base theory (Brown et al., 2005; Donaldson et al., 2005; LaCroix et al., 2018; Lin et al., 2019; Salkovskis et al., 1990; Stewart et al., 2009; Wei et al., 2013). Of these, two showed a statistically significant difference favoring intervention (Brown et al., 2005; Salkovskis et al., 1990). Nonetheless, some studies with significant differences (Gysin-Maillart et al., 2016; Hvid et al., 2011; Lahoz et al., 2016) used some Cognitive Behavioral therapy techniques. DBT was another prominent theory in four investigations (Andreasson et al., 2016; McCauley et al., 2018; Lin et al., 2019; Linehan et al., 2015). Only the study by McCauley et al. (2018) showed a difference in favor of the therapy at the first follow-up. In another systematic review of the effectiveness of psychotherapies in reducing suicidal behavior through observational studies, 40 articles were selected, of which 17 investigated the effects of the intervention on reducing suicide attempts (Méndez-Bustos et al., 2019). The results showed that 15 articles observed positive outcomes stemming from frequent weekly sessions applying DBT methods. Considering these results, CBT and DBT seem to be promising options for interventions with suicide attempts. In the systematic review by Jeong et al. (2023), which included 26 studies of patients who were treated in emergency services after suicide attempts, CBT and DBT were identified as the most promising interventions, with DBT showing better results for individuals with borderline personality disorder.
The analysis of the risk of bias in the studies showed some concerns in most studies, indicating that certain elements adopted in the study design may produce bias in the results. Although this raises some doubts regarding the quality of studies on psychotherapeutic interventions to reduce additional suicide attempts, it should be considered that the tool used for evaluation was published recently, after most of the selected studies. Furthermore, some characteristics of the psychological interventions make it difficult to blind participants and therapists, which generates bias.
The meta-analysis was carried out by comparing psychotherapy with treatment as usual. Results did not show any statistical difference between the groups in the follow-up studies within 12 months. After 12 months, the results favored the intervention group in four articles. These results highlight the medium-term effectiveness of therapeutic interventions, confirming the hypothesis that such interventions should be implemented in public health services. Nonetheless, it is important to emphasize that the results of meta-analyses in very heterogeneous psychological studies with different inclusion criteria, different forms of measurement, and different control groups must be interpreted with care (Wenzel et al., 2010). Even those studies that favored intervention show different session times and focus on different cognitive and behavioral aspects. This heterogeneity was also found in another study, which evaluated the effectiveness of CBT in reducing suicidal ideation and behavior, administered either face-to-face or online. Leavey and Hawkins (2017) concluded that there was a statistically significant small to medium effect favoring CBT face-to-face intervention for reducing suicidal ideation and behavior (including attempts and deaths by suicide), although there was significant heterogeneity between the studies considered. Suicidal patients are a heterogeneous group and this variability is not reflected in randomized clinical trials due to the required inclusion and exclusion criteria. Given this, it is also necessary to analyze observational studies. It is important to emphasize that most studies exclude patients with exacerbated psychological disorders. As such, further research with specific groups presenting severe psychotic symptoms, mania, or cognitive deficits may be useful.
Another limitation is the difference between the results from self-reporting measures, such as tests and questionnaires, and those from hospital records. This difference can be observed when considering Morthorst et al. (2012), which adopted a 12-month follow-up period. From hospital records, they found that new suicide attempts were reported for 20 out of 123 patients (16 %) in the intervention group, compared with 13 out of 120 patients (11 %) in the control group. In the same study, data from self-reporting showed that 11 out of 95 (12 %) participants in the intervention group versus 13 out of 74 (18 %) in the control group tried to commit suicide. Why do medical records show more attempts than self-reports in the intervention group and the opposite in the control group? Given this, measurement techniques for suicide attempts require further investigation and improvement for future research.
There has been a scarcity of studies using humanistic or psychoanalytic therapies. This does not mean that these types of psychotherapies are not being used in studies aimed at patients with suicidal behavior, but the hypothesis is that quantitative clinical trial methodology is not emphasized in these studies.
Some important issues are worth additional consideration. Within psychotherapy, which factor is preponderant in reducing suicide attempts? The development of strategies during moments of crisis? The work undertaken with interpersonal conflicts? The research team's sense of care? Designing and implementing higher-quality primary studies that analyze these items separately is necessary. Huggett et al. (2022), exemplify this argument. A study that evaluated the relationship between the therapeutic alliance in psychotherapy and suicidal experiences in a literature review by Huggett et al. (2022) revealed mixed evidence for the relationship between the therapeutic alliance and suicidal experiences as predictors, correlates, and outcomes. However, a strong therapeutic alliance reported at the beginning of psychotherapy was associated with a subsequent reduction in suicidal ideation and attempts. Nonetheless, replication studies are also needed to identify specific interventions that are effective in routine clinical settings.
Five studies included adolescents in their sample (McCauley et al. 2018; Morthorst et al. 2012; Salkovskis et al., 1990; van der Sande et al., 1997; Wei et al., 2013): only the study by Salkovskis et al. (1990) identified a significant difference in the first follow-up, favoring the intervention. It is recommended to distinguish age groups among participants, as specific care is needed for each group. An example of the effectiveness of a specific intervention for adolescents, which benefited female adolescents within six months of follow-up, is the PositivaMente program for suicide prevention, developed in Spain in educational settings. This program demonstrated a significant difference favoring the intervention in terms of subjective well-being, reduction of emotional problems, and peer issues in females (Díez-Gómez et al., 2024). All participants in the research by Linehan et al. (2015) were women, and the vast majority of participants with suicide attempts were female. It is important to consider the specificities of participants when developing interventions based on the specific needs of each group. Future work should address these issues of gender and age, as they may influence the development of interventions that are more likely to be effective
Suicide attempts are consequences of numerous factors, and through psychotherapy, the goal is to help the participant cope with problems, develop interpersonal and emotional skills, dismantle maladaptive beliefs and cognitive distortions, build resilience, and reframe past traumas. However, there is a vast array of risk factors that psychotherapy alone cannot address, such as situations of extreme poverty, cultural beliefs, and biological issues. Hence, there is a need for studies that encompass the complexity of these factors for suicide prevention, combining psychotherapy with other interventions within an intersectoral network.
Conclusion
This systematic review provides long-term evidence for psychotherapeutic interventions against future suicide attempts. This illustrates the importance of studies that assess the efficacy and effectiveness of psychotherapeutic interventions. The results also show the scarcity of and need for more studies on psychotherapies, with greater methodological rigor, which could generate significant beneficial outcomes for high-risk patients presenting prior suicide attempts. Additionally, psychological interventions included different strategies for suicide crisis management. Most of them tried to develop interpersonal and emotional skills and change maladaptive beliefs and cognitive distortions.
This study is a systematic review and comprehensive meta-analysis seeking to investigate effective psychotherapeutic treatments for patients who have experienced prior suicide attempts. While other systematic reviews have been carried out with sample populations presenting ideation, planning, suicide attempts, and self-mutilation with suicidal ideation (Briggs, 2019; Grupp-Phelan et al., 2019; Hepp et al., 2004; Ougrin et al., 2015; Rudd et al., 2015), this study presents specific results for patients with prior suicide attempts.
These types of studies are very important to support public health initiatives and reduce the knowledge gap surrounding treatment options for people with prior suicide attempts. This study can be employed as a tool by government agencies to ensure effective funding for the development and establishment of designated centers to treat people who seek death to relieve unbearable suffering.
Funding
Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq).
References:
Almondes, K. M., & Teodoro, M. (2020). Os três Ds: desespero, desamparo e desesperança em profissionais da saúde. Sociedade Brasileira de Psicologia. Tópico 3. https://acortar.link/7O2Es7
Andreasson, K., Krogh, J., Wenneberg, C., Jessen, H. K., Krakauer, K., Gluud, C., Thomsen, R. R., Randers, L., & Nordentoft, M. (2016). Effectiveness of dialectical behavior therapy versus collaborative assessment and management of suicidality treatment for reduction of self-harm in adults with borderline personality traits and disorder-a randomized observer-blinded clinical trial. Depression and Anxiety, 33(6), 520-530. https://doi.org/10.1002/da.22472
Arias, S. A, Miller, I., Camargo, C.A., Jr, Sullivan, A. F., Goldstein, A. B., Allen, M. H., Manton, A. P., & Boudreaux, E. D. (2016). Factors associated with suicide outcomes 12 months after screening positive for suicide risk in the emergency department. Psychiatry Serviçes, 67(2), 206-213. https://doi.org/10.1176/appi.ps.201400513
Arvilommi, P., Valkonen, J., Ruishalme, O., Kukkonen, M., Sihvola, H., Lindholm, L., Suominen, K., Gaily-Luoma, S., & Isometsä, E. (2021). A randomized clinical trial of the ASSIP vs. crisis counselling in preventing suicide attempt repetition: a two-year follow-up study. Nordic Journal of Psychiatry, 75(sup1). https://doi.org/10.1080/08039488.2021.2019916
Bertolote, J. M. (2012). O suicídio e sua prevenção. Unesp.
Botega, N. J. (2023). Crise suicida: avaliação e manejo (2nd ed). Artmed.
Brazil. Ministry of Health. (2024). Panorama of suicides and self-inflicted injuries in Brazil from 2010 to 2021. Epidemiological Bulletin, 55(4), 1-18.
Briggs, S., Netuveli, G., Gould, N., Gkaravella, A., Gluckman, N. S., Kangogyere, P., Farr, R., Goldblatt, M. J., & Lindner, R. (2019). The effectiveness of psychoanalytic/psychodynamic psychotherapy for reducing suicide attempts and self-harm: systematic review and meta-analysis. The British Journal of Psychiatry, 214(6), 320-328. https://doi.org/10.1192/bjp.2019.33
Brown, G. K., Ten Have, T., Henriques, G. R., Xie, S. X., Hollander, J. E., & Beck, A. T. (2005). Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA, 294(5), 563-570. https://doi.org/10.1001/jama.294.5.563
Center for Disease Control and Prevention. (2016). WISQARS: Web-based injury Statistics Query and Reporting System. https://wisqars.cdc.gov/
Cuijpers, P., de Beurs, D. P., Van Spijker, B. A., Berking, M., Andersson, G., & Kerkhof, A. J. (2013). The effects of psychotherapy for adult depression on suicidality and hopelessness: a systematic review and meta-analysis. Journal of Affective Disorders, 144(3), 183-190. https://doi.org/10.1016/j.jad.2012.06.025
Díez-Gómez, A., Sebastián-Enesco, C., Pérez-Albéniz, A., Lucas-Molina, B., Al-Halabí, S., & Fonseca-Pedrero, E. (2024). The PositivaMente Program: universal prevention of suicidal behaviour in educational settings. School Mental Health, 16, 455-466. https://doi.org/10.1007/s12310-024-09650-0
Donaldson, D., Spirito, A., & Esposito-Smythers, C. (2005). Treatment for adolescents following a suicide attempt: results of a pilot trial. Journal of the American Academy of Child & Adolescent Psychiatry, 44(2), 113-120. https://doi.org/10.1097/00004583-200502000-00003
Fonseca-Pedrero, E., Pérez-Álvarez, M., Al-Halabí, S., Inchausti, F., Muñiz, J., López-Navarro, E., Pérez de Albéniz, A., Lucas Molina, B., Debbané, M., Bobes-Bascarán, M. T., Gimeno-Peón, A., Prado-Abril, J., Fernández-Álvarez, J., Rodríguez-Testal, J. F., González Pando, D., Díez-Gómez, A., García Montes, J. M., García Cerdán, L., Osma, J., ... & Ma, R. J. (2021b). Tratamientos psicológicos empíricamente apoyados para adultos: Una revisión selectiva. Psicothema, 33(2), 188-197. https://doi.org/10.7334/psicothema2020.426
Grupp-Phelan, J., Stevens, J., Boyd, S., Cohen, D. M., Ammerman, R. T., Liddy-Hicks, S., Heck, K., Marcus, S. C., Stone, L., Campo, J. V., & Bridge, J. A. (2019). Effect of a motivational interviewing-based intervention on initiation of mental health treatment and mental health after an emergency department visit among suicidal adolescents: A randomized clinical trial. JAMA Network Open, 2(12), e1917941. https://doi.org/10.1001/jamanetworkopen.2019.17941
Gysin-Maillart, A., Schwab, S., Soravia, L., Megert, M., & Michel, K. (2016). A novel brief therapy for patients who attempt suicide: A 24-months follow-up randomized controlled study of the Attempted Suicide Short Intervention Program (ASSIP). PLoS Medicine, 13(3), e1001968. https://doi.org/10.1371/journal.pmed.1001968
Hassanzadeh M., Khajeddin, N., Nojomi, M., Fleischmann, A., & Eshrati, T. (2010). Brief intervention and contact after deliberate self-harm: an Iranian randomized controlled trial. Iran Journal of Psychiatry and Behavior Sciences, 4(2), 5-12.
Hepp, U., Wittmann, L., Schnyder, U., & Michel, K. (2004). Psychological and psychosocial interventions after attempted suicide: an overview of treatment studies. Crisis, 25(3), 108-117. https://doi.org/10.1027/0227-5910.25.3.108
Higgins, J. P. T., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ, 327, 557-560. https://doi.org/10.1136/bmj.327.7414.557
Huggett, C., Gooding, P., Haddock, G., Quigley, J., & Pratt, D. (2022). The relationship between the therapeutic alliance in psychotherapy and suicidal experiences: A systematic review. Clinical Psychology & Psychotherapy, 29(4), 1203-1235. https://doi.org/10.1002/cpp.2726
Hvid, M., Vangborg, K., Sørensen, H. J., Nielsen, I. K., Stenborg, J. M., & Wang, A. G. (2011). Preventing repetition of attempted suicide—II. The Amager Project, a randomized controlled trial. Nordic Journal of Psychiatry, 65(5), 292-298. https://doi.org/10.3109/08039488.2010.544404
Inagaki, M., Kawashima, Y., Yonemoto, N., & Yamada, M. (2019). Active contact and follow-up interventions to prevent repeat suicide attempts during high-risk periods among patients admitted to emergency departments for suicidal behavior: a systematic review and meta-analysis. BMC Psychiatry, 19, 44. https://doi.org/10.1186/s12888-019-2017-7
Jeong, H., Yim, H. W., Lee, S. Y., Potenza, M. N., & Kim, N. J. (2023). Effectiveness of psychotherapy on prevention of suicidal re-attempts in psychiatric emergencies: a systematic review and network meta-analysis of randomized controlled trials. Psychotherapy and Psychosomatics, 92(3), 152-161. https://doi.org/10.1159/000529753
Labelle, R., Pouliot, L., & Janelle, A. (2015). A systematic review and meta-analysis of cognitive behavioural treatments for suicidal and self-harm behaviours in adolescents. Canadian Psychology, 56(4), 368-378. https://doi.org/10.1037/a0039159
LaCroix, J. M., Perera, K. U., Neely, L. L., Grammer, G., Weaver, J., & Ghahramanlou-Holloway, M. (2018). Pilot trial of post-admission cognitive therapy: Inpatient program for suicide prevention. Psychological Services, 15(3), 279-288. https://doi.org/10.1037/ser0000224
Lahoz, T., Hvid, M., & Wang, A. G. (2016). Preventing repetition of attempted suicide-III. The Amager Project, 5-year follow-up of a randomized controlled trial. Nordic Journal of Psychiatry, 70(7), 547-553. https://doi.org/10.1080/08039488.2016.1180711
Leavey, K., & Hawkins, R. (2017). Is cognitive behavioural therapy effective in reducing suicidal ideation and behaviour when delivered face-to-face or via e-health? A systematic review and meta-analysis. Cognitive Behaviour Therapy, 46(5), 353-374. https://doi.org/10.1080/16506073.2017.1332095
Lin, T-J., Ko, H-C., Wu, J. Y-W, Oei, T. P., Lane, H-Y., & Chen, C-H. (2019). The Effectiveness of Dialectical Behavior Therapy skills training group vs. Cognitive Therapy group on reducing depression and suicide attempts for borderline personality disorder in Taiwan. Archives of Suicide Research, 23(1), 82-99. https://doi.org/10.1080/13811118.2018.1436104
Linehan, M. M. (2018). Skills training in DBT: Dialectical behavior therapy manual for the therapist (2nd ed.). Artmed.
Linehan, M. M., Korslund, K. E., Harned, M. S., Gallop, R. J., Lungu, A., Neacsiu, A. D., McDavid, J., Comtois, K. A., & Murray-Gregory, A. M. (2015). Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: a randomized clinical trial and component analysis. JAMA Psychiatry, 72(5), 475-482. https://doi.org/10.1001/jamapsychiatry.2014.3039
Macedo, M. M. K., & Werlang, B. S. G. (2004). Trauma, pain, and act: The psychoanalytic perspective on a suicide attempt. Ágora, 10(1), 86-106. https://doi.org/10.1590/S1516-14982007000100006
Malakouti, S. K., Nojomi, M., Ghanbari, B., Rasouli, N., Khaleghparast, S., & Farahani, I. G. (2022). Aftercare and suicide reattempt prevention in Tehran, Iran. Crisis, 43(1), 18-27. https://doi.org/10.1027/0227-5910/a000754
McCauley, E., Berk, M. S., Asarnow, J. R., Adrian, M., Cohen, J., Korslund, K., Avina, C., Hughes, J., Harned, M., Gallop, R., & Linehan, M. M. (2018). Efficacy of dialectical behavior therapy for adolescents at high risk for suicide: A randomized clinical trial. JAMA Psychiatry, 75(8), 777-785. https://doi.org/10.1001/jamapsychiatry.2018.1109
Méndez-Bustos, P., Calati, R., Rubio-Ramírez, F., Olié, E., Courtet, P., & Lopez-Castroman, J. (2019). Effectiveness of psychotherapy on suicidal risk: a systematic review of observational studies. Frontiers in Psychology, 10, 277. https://doi.org/10.3389/fpsyg.2019.00277
Messiah, A., Notredame, C. E., Demarty, A. L., Duhem, S., Vaiva, G., & AlgoS investigators. (2019). Combining green cards, telephone calls and postcards into an intervention algorithm to reduce suicide reattempt (AlgoS): P-hoc analyses of an inconclusive randomized controlled trial. PloS One, 14(2), e0210778. https://doi.org/10.1371/journal.pone.0210778
Morthorst, B., Krogh, J., Erlangsen, A., Alberdi, F., & Nordentoft, M. (2012). Effect of assertive outreach after suicide attempt in the AID (Assertive Intervention for Deliberate Self harm) trial: randomised controlled trial. BMJ, 345, e4972 https://doi.org/10.1136/bmj.e4972
Mousavi, S. G., Amini, M., Mahaki, B., & Bagherian-Sararoudi, R. (2016). Effect of phone call versus face-to-face follow-up on recurrent suicide attempts prevention in individuals with a history of multiple suicide attempts. Advanced Biomedical Research, 5, 184. https://doi.org/10.4103/2277-9175.190990
Nock, M. K., Borges, G., Bromet, E. J., Cha, C. B., Kessler, R. C., & Lee, S. (2008). Suicide and suicidal behavior. Epidemiologic Reviews, 30(1), 133-154. https://doi.org/10.1093/epirev/mxn002
Ougrin, D., Tranah, T., Stahl, D., Moran, P., & Asarnow, J. R. (2015). Therapeutic interventions for suicide attempts and self-harm in adolescents: systematic review and meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 54(2), 97-107. https://doi.org/10.1016/j.jaac.2014.10.009
Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan—a web and mobile app for systematic reviews. Systematic Reviews, 5, 210 https://doi.org/10.1186/s13643-016-0384-4
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., & Moher, D. (2021). Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. Journal of Clinical Epidemiology, 134, 103-112. https://doi.org/10.1016/j.jclinepi.2021.02.003
Probert-Lindström, S., Berge, J., Westrin, Å., Öjehagen, A., & Skogman Pavulans, K. (2020). Long-term risk factors for suicide in suicide attempters examined at a medical emergency in patient unit: results from a 32-year follow-up study. BMJ Open, 10(10), e038794. https://doi.org/10.1136/bmjopen-2020-038794
Rodrigues, C. L., & Ziegelmann, P. K. (2010). Metanálise: um guia prático. Clinical & Biomedical Research, 30(4), 436-447.
Roever, L. (2016). Compreendendo os estudos de metanálise na pesquisa clínica. Revista da Sociedade Brasileira de Clínica Médica, 14(4), 245-250.
Rogers, C. R. (1995). On Becoming a Person: A Therapist’s view of psychotherapy. Houghton Mifflin.
Rudd, M. D., Bryan, C. J., Wertenberger, E. G., Peterson, A. L., Young-McCaughan, S., Mintz, J., Williams, S. R., Arne, K. A., Breitbach, J., Delano, K., Wilkinson, E., & Bruce, T. O. (2015). Brief cognitive-behavioral therapy effects on post-treatment suicide attempts in a military sample: results of a randomized clinical trial with 2-year follow-up. The American Journal of Psychiatry, 172(5), 441-449. https://doi.org/10.1176/appi.ajp.2014.14070843
Salkovskis, P. M., Atha, C., & Storer, D. (1990). Cognitive-behavioural problem solving in the treatment of patients who repeatedly attempt suicide a controlled trial. The British Journal of Psychiatry, 157(6), 871-876. https://doi.org/10.1192/bjp.157.6.871
Santos, C. M. C, Pimenta, C. A. M., & Nobre, M. R. C. (2007). The PICO strategy for the research question construction and evidence search, updating articles. Revista Latino-Americana de Enfermagem, 15(3), 1-4. https://doi.org/10.1590/S0104-11692007000300023
Shneidman, E. S. (1993). Suicide as psychache: A clinical approach to self-destructive behavior. Jason Aronson.
Silverman, M. M. (2006). The language of suicidology. Suicide and Life-Threatening Behaviour, 36(5), 519-532. https://doi.org/10.1521/suli.2006.36.5.519
Sterne, J. A. C., Savović, J., Page, M. J., Elbers, R.G., Blencowe, N. S., Boutron, I., Cates, C. J., Cheng H-Y., Corbett, M. S., Eldridge, S. M., Emberson J. R., Hernán, M. A., Hopewell, S., Hróbjartsson, A., Junqueira, D. R., Jüni, P., Kirkham, J. J., Lasserson, T., Li T., … Higgins, J. P. T. (2019). RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ, 366, l4898. https://doi.org/10.1136/bmj.l4898
Stewart, C. D., Quinn, A., Plever, S., & Emmerson, B. (2009). Comparing cognitive behavior therapy, problem solving therapy, and treatment as usual in a high risk population. Suicide and Life-Threatening Behavior, 39(5), 538-547. https://doi.org/10.1521/suli.2009.39.5.538
Torre-Luque, A., Estupiñá Puig, F. J., Pemauy, A., & Prata, J. (2021). General strategies for suicide behavior prevention. In S. Al-Halabí & E. Fonseca-Pedrero (Eds.), Manual of psychology of suicidal behavior (pp. 173-193). Pirámide.
van der Sande, R., Van Rooijen, L., Buskens, E., Allart, E., Hawton, K., Van der Graaf, Y., & Van Engeland, H. (1997). Intensive in-patient and community intervention versus routine care after attempted suicide. A randomised controlled intervention study. The British Journal of Psychiatry, 171(1), 35-41. https://doi.org/10.1192/bjp.171.1.35
Wang, Y. C., Hsieh, L. Y., Wang, M. Y., Chou, C. H., Huang, M. W., & Ko, H. C. (2016). Coping card usage can further reduce suicide reattempt in suicide attempter case management within 3-month intervention. Suicide and Life-Threatening Behavior, 46(1), 106-120. https://doi.org/10.1111/sltb.12177
Wei, S., Liu, L., Bi, B., Li, H., Hou, J., Tan, S., Chen, X., Chen, W., Jia, X., Dong, G., Qin, X., & Liu, Y. (2013). An intervention and follow-up study following a suicide attempt in the emergency departments of four general hospitals in Shenyang, China. Crisis, 34(2), 107-115. https://doi.org/10.1027/0227-5910/a000181
Wenzel, A., Brown, G. K., & Beck, A. T. (2010). Terapia cognitivo-comportamental para pacientes suicidas. Artmed.
World Health Organization. (2014). Preventing suicide: a global imperative. http://www.who.int/mental_health/suicide-prevention/en/.
World Health Organization. (2019). Suicide in the world: Global health estimatives. https://apps.who.int/iris/bitstream/handle/10665/326948/WHO-MSD-MER-19.3-eng.pdf?sequence=1&isAllowed=y
Data availability: The dataset supporting the results of this study is not available.
How to cite: Santos, L. A., Teodoro, M. L. M., & De Oliveira, F. C. (2024). The effectiveness of psychotherapies in reducing further suicide attempts: a systematic review with meta-analysis of randomized controlled trials. Ciencias Psicológicas, 18(2), e-3667. https://doi.org/10.22235/cp.v18i2.3667
Authors’ contribution (CRediT Taxonomy): 1. Conceptualization; 2. Data curation; 3. Formal Analysis; 4. Funding acquisition; 5. Investigation; 6. Methodology; 7. Project administration; 8. Resources; 9. Software; 10. Supervision; 11. Validation; 12. Visualization; 13. Writing: original draft; 14. Writing: review & editing.
L. A. S. has contributed in 1, 2, 3, 5, 6, 7, 8, 9, 11, 12, 13, 14; M. L. M. T. in 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14; F. C. O. in 2, 3, 5, 6, 9, 11, 12, 13.
Scientific editor in-charge: Dr. Cecilia Cracco.
Appendix A
Table A1: Database: PubMed
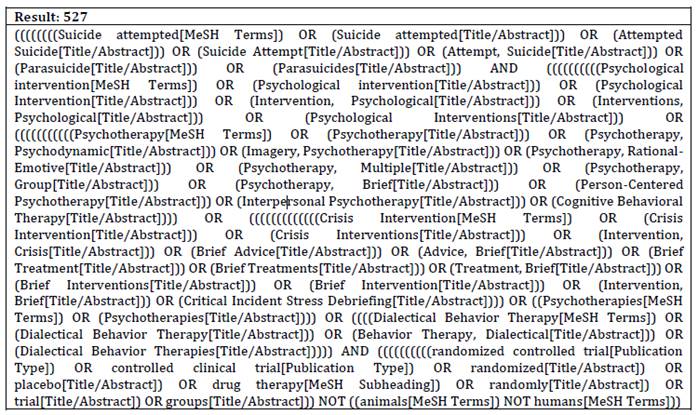
Table A2: Database: Cochrane
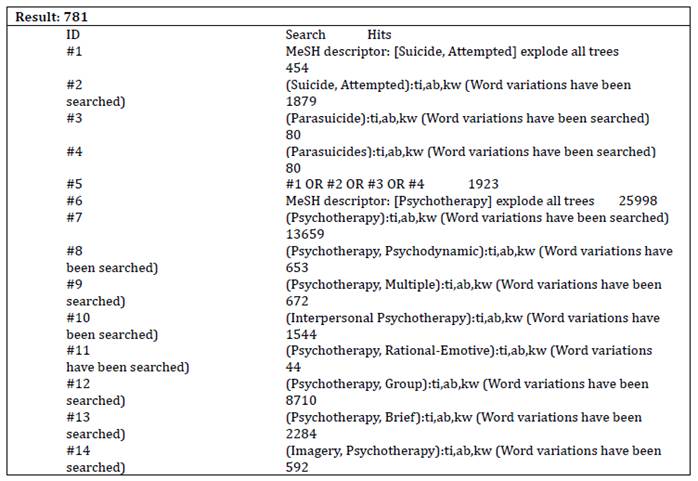
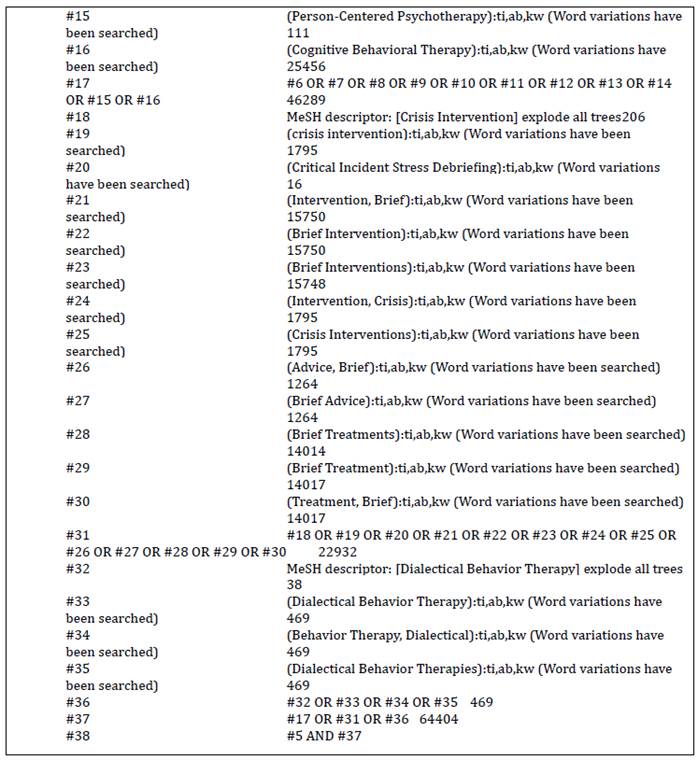
Table A3: Database: APA PsycInfo
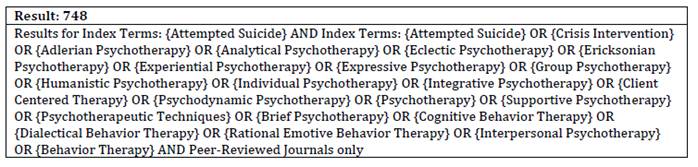
Table A4: Database: LILACS