10.22235/cp.v17i2.3009
Psychometric properties of the Measurement of Current Status (MOCS) Scale in Mexican cancer patients
Propiedades psicométricas de la Escala de Medida del Estado Actual (MOCS) en pacientes mexicanos con cáncer
Propriedades psicométricas da Escala de Medida do Estado Atual (MOCS) em pacientes mexicanos com câncer
Marcos Espinoza Bello1, ORCID 0000-0003-3090-8098
Oscar Galindo Vázquez2, ORCID 0000-0001-9395-2921
Frank J. Penedo3, ORCID 0000-0002-2780-0417
Miguel Ángel Jiménez Ríos4, ORCID 0000-0002-2231-1921
Patricia Ortega Andeane5, ORCID 0000-0002-2780-0417
Anna Scavuzzo6, ORCID 0000-0001-9558-8086
Mirna García Méndez7, ORCID 0000-0002-2334-0740
Abelardo Meneses-García8, ORCID 0000-0003-4032-4598
1 Uni Instituto Nacional de Cancerología, Universidad Nacional Autónoma de México, [email protected]
2 Instituto Nacional de Cancerología, Mexico
3 University of Miami, United States
4 Instituto Nacional de Cancerología, Mexico
5 Universidad Nacional Autónoma de México, Mexico
6 Instituto Nacional de Cancerología, Mexico
7 Universidad Nacional Autónoma de México, Mexico
8 Instituto Nacional de Cancerología, Mexico
Abstract:
Background: Cancer is a public health problem, and stress is one of the psychosocial variables associated to this disease, which calls for the need to have a reliable scale to measures stress in the Hispanic population with cancer. Objective: To determine the psychometric properties of the Measurement of Current Status (MOCS) Scale in Mexican cancer patients. Method: Study design: Cross-sectional, non-experimental instrumental. A total of 197 patients aged 18-81 years, at any clinical stage, receiving cancer treatment or follow-up were included. Instruments: MOCS and emotional distress thermometer. Statistical analysis: Confirmatory factor analysis was performed to evaluate the fit of the model to the data using the maximum likelihood estimation and cut-off points. Results: Two models were obtained. The first, self-perceived current state, had an alpha of .90 with an explained variance of 74.2 %; the second, non-specific effect, with an alpha of .61 and an explained variance of 74.3 %. The confirmatory factor analysis showed that both models had indexes suggesting stability and acceptable adjustment. Scores are shown by interquartile ranges for each model. Conclusions: The Mexican version of the MOCS is reliable and valid; with a confirmatory factor structure similar to the original version. Therefore, we support its use in the clinical and research setting with cancer patients.
Keywords: stress; cancer; psychological tests; Mexico; validation study.
Resumen:
Antecedentes: El cáncer es un problema de salud pública, una de las variables psicosociales en relación con esta enfermedad es el estrés, por tanto es necesario tener una escala que mida el estrés en población hispana con cáncer. Objetivo: Determinar las propiedades psicométricas de la Escala de Medida del Estado Actual (MOCS, por sus igla en inglés) en pacientes mexicanos con cáncer. Método: Estudio transversal, instrumental no experimental. Participaron 197 pacientes de 18 a 81 años, de cualquier etapa clínica, en tratamiento o seguimiento del cáncer. Instrumentos: MOCS y termómetro de malestar emocional. Análisis estadísticos: análisis factorial confirmatorio para evaluar el ajuste del modelo a los datos mediante el método de máxima verosimilitud y puntos de corte. Resultados: Se obtuvieron dos modelos, el primero, estado actual autopercibido, con un alfa de .90 varianza explicada de 74.2 %, el segundo, efectos inespecíficos, con un alfa de .61 varianza explicada de 74.3 %. El análisis factorial confirmatorio mostró que ambos modelos tuvieron índices que sugieren estabilidad, ajuste aceptable, se muestran puntajes mediante rangos intercuartílicos para cada modelo. Conclusiones: la versión mexicana del MOCS tiene confiabilidad y validez, su estructura factorial confirmatoria es similar a la versión original. Se recomienda su uso en la práctica clínica e investigación en pacientes con cáncer.
Palabras clave: estrés; cáncer; pruebas psicológicas; México; estudio de validación.
Resumo:
Antecedentes: O câncer é um problema de saúde pública, uma das variáveis psicossociais relacionadas a essa doença é o estresse, portanto, é necessário ter uma escala que meça o estresse na população hispânica com câncer. Objetivo: Determinar as propriedades psicométricas da Escala de Medição do Estado Atual (MOCS) em pacientes mexicanos com câncer. Método: Desenho do estudo: transversal, instrumental, não experimental. Participaram 197 pacientes com idades entre 18 e 81 anos, em qualquer estágio clínico, em tratamento ou acompanhamento do câncer. Instrumentos: MOCS e Termômetro de desconforto emocional. Análises estatísticas: análise fatorial confirmatória para avaliar o ajuste do modelo aos dados por meio do método de máxima verossimilhança e pontos de corte. Resultados: Foram obtidos dois modelos, o primeiro estado atual autopercebido com um alfa de 0,90 variância explicada de 74,2 %, o segundo efeito inespecífico com um alfa de 0,61 variância explicada de 74,3 %; a análise fatorial confirmatória mostrou que ambos os modelos tiveram índices que sugerem estabilidade, ajuste aceitável e são demonstradas pontuações por meio de intervalos interquartis para cada modelo. Conclusões: a versão mexicana do MOCS tem confiabilidade e validade; sua estrutura fatorial confirmatória é semelhante à versão original. É recomendado para prática clínica e pesquisa em pacientes com câncer.
Palavras-chave: estresse; câncer; testes psicológicos; México; estudo de validação.
Received: 30/08/2022
Accepted: 22/08/2023
In 2020, 19,292,789 cases of cancer were reported worldwide. Breast cancer was the most prevalent with 2,261,419 (11.7 %), followed by lung cancer with 2,206,771 (11.4 %) and prostate cancer with 1,414,259 (7.3 %). In the same year, the number of deaths from this disease amounted to 9,958,133. In Latin America, 1,470,274 cases were reported. Prostate cancer ranked first with 214,522 (14.6 %), followed by breast cancer 210,100 (14.3 %) and colorectal cancer 134,943 (9.2 %). The number of deaths due to cancer in this region was 713,414 (Chhikara & Parang, 2023; Sung et al., 2021).
In Mexico, 195,499 cases were estimated in 2020. The cancer with the highest incidence was breast cancer with 29,929 (15.3 %), followed by prostate cancer with 26,742 (13.7 %), and colorectal cancer with 14,901 (7.6 %). The number of deaths was estimated at 89,5361 (Sung et al., 2021). In Mexico, cancer is the third leading cause of death, after cardiovascular diseases and diabetes (Sociedad Mexicana de Oncología, 2016).
Patients with cancer also experience different psychosocial issues, including stress that can be present during the diagnosis, treatment and follow-up period (Kang et al., 2012). Perceived stress is defined as the feelings or thoughts that individuals have about how much stress they are dealing with at any given moment. It includes feelings about the uncontrollability and unpredictability of life, how often the individual has to deal with distressing situations, how much changes are occurring in their life, and the confidence in their own ability to cope with these problems or difficulties (Lazarus & Folkman, 1984).
In cancer patients, stress is quite prevalent with 18.9 % to 66.3 % reporting moderate stress levels. Also, 20-30 % report severe stress a year after diagnosis, and 74 % report a stressful experience after diagnosis and surgery (Bleiker et al., 2000; Golden-Kreutz & Andersen, 2004; Haugland et al., 2016).
Several instruments have been used to measure stress in cancer patients, such as the Perceived Stress Scale with a test-retest reliability of .65 to .74 (Fernández Seara & Nielgo Robles, 1996), the Perceived Stress Questionnaire, with an alpha of .90 (Levenstein et al., 1993), and the Impact of Event Scale, with alphas of .78 to .82 (Horowitz et al., 1979). These scales, have acceptable psychometric properties but were not designed specifically for oncologic settings nor to identify the effects of psychosocial interventions.
The Measurement of Current Status Scale (MOCS, Carver, 2006) has been designed to measure perceived stress specifically for this population and has been used to measure the effects of clinical interventions such as cognitive behavioral therapy (CBT). This scale derives from part of the assessment of the psychosocial well-being of breast cancer patients and was created to answer whether the beneficial effects of the intervention have multiple sources or if there is a single component and to investigate the possible “active components” behind the intervention’s effects (Carver, 2006). It has subsequently been used in other clinical research with cancer patients (Antoni et al., 2006; Penedo et al., 2006; Phillips et al., 2012).
There is a pending need to have specific, valid, and reliable instruments to assess the psychosocial aspects of cancer patients, including stress, also it is important to know how these variables are modified by treatment with CBT. This will help to have a more accurate understanding about these variables in the Hispanic population and to be able to offer treatment tailored to the patient’s needs. The aim of the present study was to determine the psychometric properties of the Measurement of Current State (MOCS) Scale in a sample of Mexican cancer patients.
Method
This study had cross-sectional, instrumental, non-experimental design (Carretero-Dios & Pérez, 2005). A total of 197 Mexican participants with cancer were included, they were selected by non-probabilistic sampling (Table 1).
Table 1: Sociodemographic data of the participants
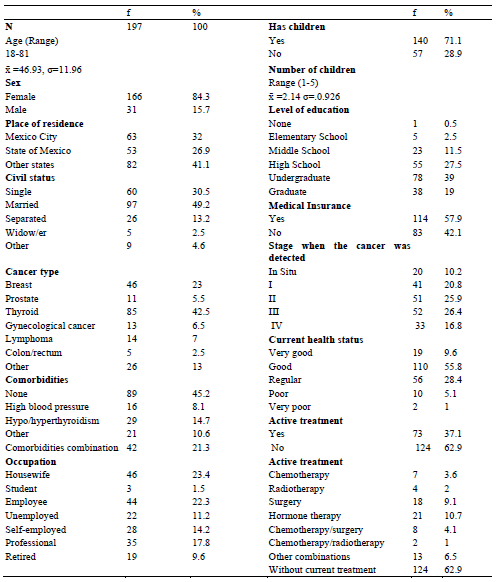
Inclusion criteria of participation: Any oncologic diagnosis, 18 years or older, in any type or combination of treatments or follow-up period, any clinical stage, able to read and write, and who agreed to participate after reading the informed consent. Exclusion criteria of participation: non-Mexican nationality, psychiatric diagnosis informed by the patient. Elimination criteria: the participant deciding not to continue participating, incomplete instruments.
Instruments
Measurement of Current State (MOCS) Scale. The MOCS scale developed by Carver (2006) contains 23 items divided into two sections (Antoni et al., 2006). Section A has 13 items that evaluate the self-perceived current state. For the ratings, a Likert-type scale ranging from “I cannot do this at all” (0) to “I can do this extremely well” (4). The scale has individual alphas ranging from .71 to .89, with four factors. The factors are: 1) the ability to relax at will: reducing the state of physiological activation, facilitating the recovery of calm, mental balance and a sense of inner peace, and its effects on physiological, emotional, cognitive and behavioral processes (Ruiz Fernández et al., 2012); 2) recognizing situations that cause stress: the particular relationship between the individual and his/her environment, the latter is evaluated by the subject as threatening or surpassing his resources and its capacity to endanger his/her well-being (Lazarus & Folkman, 1984); 3) restructuring maladaptive thoughts: the individual identifies, evaluates and modifies maladaptive thoughts, appraisals and beliefs (Dobson & Dozois, 2010); 4) being assertive about their needs: adaptive communication style in which individuals express their feelings and needs directly, while maintaining respect for others (American Psychological Association, 2020a) and using appropriate coping responses; this is defined as the way in which people detect, evaluate, deal with and learn from stressful situations (Skinner & Zimmer-Gembeck, 2016).
Section B includes 10 items to evaluate non-specific effects. It has a Likert-type scale ranging from Strongly Disagree (0) to Strongly Agree (4) with alphas of .77 to .85 and four factors, 1) feelings of normalcy versus alienation: the comparison between the ability to think and act in an organized and reasonably effective manner versus a deep sense of dissatisfaction with one’s personal existence and a lack of confidence in one’s social or physical environment (American Psychological Association, 2020b, 2020c); 2) sense of cohesion with others: the ties that bind members to the group as a whole, the sense of belonging and community within the group, feelings of attraction to specific members of the group, and the group itself as experienced by individuals (American Psychological Association, 2020d); 3) perceptions of attention from those around them: expressive activities in which trusting relationships are established and support is offered, instrumental activities include physical and cognitive action-oriented helping behaviors (Papastavrou et al., 2011); and 4) feelings of being better off than other cancer patients: this is a form of emotional coping in people with low levels of subjective well-being that can help them feel better in the short term (Pomery et al., 2012).
Emotional Distress Thermometer. Visual analog scale of Emotional Distress (Roth et al., 1998) it was developed in 1998 and was validated for the Mexican population (Almanza et al., 2008). It consists of two parts: the first one is a visual analog scale ranging from 0 to 10, to assess the emotional distress experienced in the last week. The second section is a checklist with 35 items, in which patients mark the presence or absence of any problem in the last week. The convergent validity through the ROC analysis showed an area under the curve of .63, a sensitivity of 93 %, a specificity of 76 %, a positive predictive value of 82 %, and a negative predictive value of 90 %, with a cut-off point of 4 or more, and it has widely been used in other studies (Holland et al., 2013). Only the visual-analogue part of the thermometer was used in this study.
Procedure and data analysis
Cultural adaptation. The scale used in this validation was obtained from the Carver (2006) version, it was sent to an independent translator to obtain this Spanish version. This version was submitted to expert judgment by five psychologists with bachelor, master, or doctorate degrees, who proposed modifications on the wording of the instructions to make it more understandable for the population. Also, in part A, items 4, 10, 12 and 13; and in part B items 1 and 6; and the response options for both sections had wording modifications without losing the original sense of the English original version. A pilot test was then carried out with 12 patients to determine whether the instructions were clear, if there was any difficulty in answering, the comprehension of each item and finally to identify any offensive language (Mora et al., 2013). No modifications were made.
This version was sent to a second translator to be retranslated into English. The scale was sent to one of the principal investigators of the MOCS scale in English-speaking cancer patients and was approved. The definitive version was applied online to patients through an invitation to participate on the Google forms platform from December 2020 to May 2021. Each participant agreed to participate after reading and understanding the informed consent. This investigation complied with norms established by Mexico’s Ministry of Health, the Regulations of the General Health Law on Research, and the Helsinki Declaration on ethical principles for medical research involving human subjects. This research was approved by the ethics and research committee of the Mexico´s National Institute of Cancer (INCan) with approval INCAN/CI/394/2021.
Data analysis. A descriptive analysis was performed for each item to discard extreme data. In addition to identifying missing data, internal consistency coefficient was analyzed with an expected Cronbach’s alpha ≥ .60 (Hair et al., 1999). The explained variance of the scale was estimated, using the version 24 of the IBM SPSS® software.
Confirmatory Factor Analysis (CFA). The confirmatory factor analysis evaluated the four-factor model fit for self-perceived current state (model A) and for non-specific effects (model B) respectively with the maximum likelihood method, using the AMOS® statistical software (version 24) to estimate the data using the global fit indexes, the absolute chi-squared value (CMIN) and then the chi-squared ratio/degrees of freedom (CMIN/df) to confirm if there were null errors in the variances and covariances. The overall fit versus a null model was estimated using the Comparative Fit Index (CFI), parsimony and model balance with the Tucker-Lewis index (TLI), in addition the Root Mean Square Error of Approximation (RMSEA) was used to determine if there is a good fit of the model. Finally, the ratification of goodness of fit was obtained by calculating the standardized root mean squared residual (SRMR; Byrne, 2010; Kline, 2016). For convergent validity between MOCS and the Emotional Distress Thermometer, the Pearson’s correlation was used given the interval level of the variables with p < .05. Once these results were obtained, the Kolgomorov-Smirnov test was performed with the total sum of the items in each model to evaluate the normality of the data, and the median and interquartile ranges were used to establish cut-off points.
Results
For part A (current self-perceived status), an internal consistency of .90 (standardized Cronbach’s alpha), and an explained variance of 74.2 % was found with four factors: 1) Recognizing stress-inducing situations α = .73, 2) Being assertive about needs α = .86, 3) Choosing appropriate coping responses as needed α = .90 and 4) Ability to relax at will α = .51.
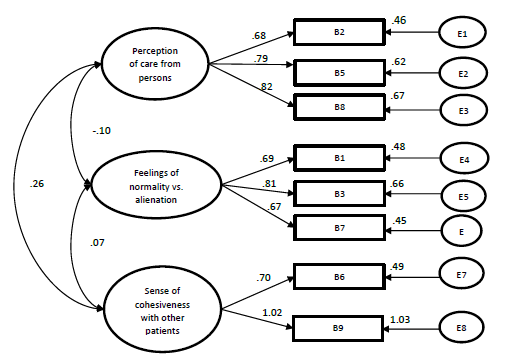
For part B (nonspecific effects) an internal consistency of .61 (standardized Cronbach’s alpha), and an explained variance of 74.3 % was found with three factors: 1) Feelings of normalcy vs. alienation α = .76, 2) Perception of care from persons around them α = .79 and 3) Sense of cohesiveness with other patients α = .83. One factor, Sense of being better off than other cancer patients α = .32 was removed because the alpha level was not satisfactory (Taber, 2018).
Confirmatory factor analysis
Figure 1 shows the model for each section (four factors), the estimators calculated for each factor, and the correlations between them, as well as the variance explained by each item. The comparative fit indices CFI = .941, and the Tucker Lewis index TLI = .920, showed fit to the data (≥ .90), a goodness of fit or Chi-normed CMIN/gl = 2.41, an RMSEA = .085, and finally, an SRMR = .0614 (< .080) (Manzano Patiño, 2017). The model A presented levels of fit to the data that support the confirmatory factor structure.
Figure 2 shows the model (three factors), the estimators calculated for each factor, and the correlations between them, as well as the variance explained by each item. The comparative fit indices (CFI = .986, TLI = .976) showed a fit to the data, a goodness of fit of CMIN = 1.417 and a RMSEA = .046. Finally, they showed a SRMR = .0401. Model B presented levels of fit to the data that support its confirmatory factorial structure.
The concurrent validity of the MOCS with the Emotional Distress Thermometer was estimated. Correlations were found to be negative, low to moderate, and statistically significant. The following Pearson’s r values were obtained: Ability to relax at will: ‑.295, Recognizing situations that provoke stress: -.226, Assertiveness about needs: -.365, Choice of coping responses: -.462, Perception of attention from other people and Feeling of cohesion with others: -.223 (p < .01 and p < .05). On the other hand, there were positive correlations between Feelings of Normality and Emotional Distress: .238 (p < .01).
The total scores of the items in both models were non-normal. Therefore, we decided to take the median and the interquartile ranges to consider cut-off points. For MOCS A (self-perceived current state), a low score was of 0-23, a medium low score was of 24-30, a medium high score was of 31-35, and a high score was of 36-52. For MOCS B (nonspecific effects), a low score was of 0-18, a medium low score was of 19-21, a medium high score was of 22-24, and a high score was of 25-32.
Figure 1: Model A (current self-perceived status)
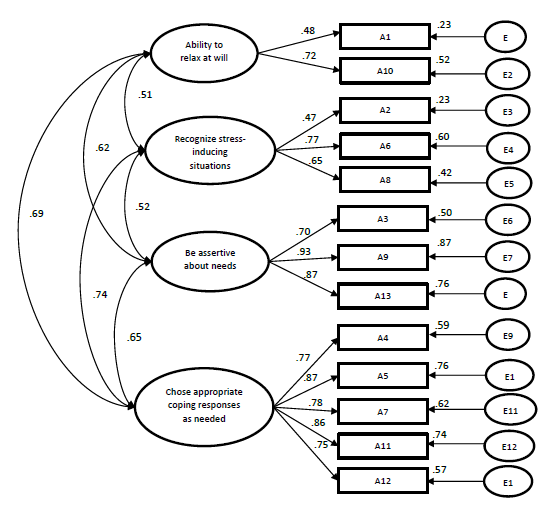
Figure 2: Model B (nonspecific effects)
Discussion
This report is the first to present information on the validity and reliability of the MOCS in Hispanic cancer patients. The aim was to provide evidence of this scale at an international level. The MOCS is a scale suitable for measuring the current self-perceived state of stress and it can measure the effects of psychosocial interventions in cancer patients. The evaluation of stress in this population is important because the evidence suggests a relationship between it and adverse health effects such as immune system impairment and inflammatory response during cancer treatment (Dai et al., 2020; Moreno-Smith et al., 2010).
The total internal consistency and by factor of section A, and the explained variance were adequate and similar to the original (Antoni et al., 2006), except for the indicator “ability to relax at will” which had a sufficient alpha according to Taber (2018).
On the other hand, the total internal consistency and by factor of section B were moderate and the independent alpha by factor was similar to the original, however, the indicator “Sense of being better off than other cancer patients” was not satisfactory and was therefore eliminated.
As said, this scale it is suggested as a means to evaluate the effect of cognitive-behavioral intervention protocols in which stress is a dependent variable, as a way to assess the active components in patients undergoing psychological treatment. Also, the explained variance levels were high in both parts of the instrument. Thus, it is suggested they may be applied in the clinical setting. Although items 4 “I'm better off than most people who have cancer” and 10 “Most people who have cancer have life a lot harder than I do” were not considered for scoring due to their low reliability, we suggest keeping them, considering their importance at a clinical level from a social perspective in terms of how the person sees him/herself in relation to others.
In the case of the CFA, the results suggest a factorial structure similar to the original version in both models. Four factors were identified for section A, and three factors for section B, with goodness of fit indexes that were reported. This provides evidence of the psychometric quality of the instrument.
Both sections have the function of identifying perceived stress, in addition to the effect of CBT on the reports of patients receiving such treatment. For this analysis, the number of participants was adequate, as shown by the confirmatory factor analysis data. However, the alpha of the MOCS B could be insufficient.
The concurrent validity of the instrument resulted in low, negative and significant correlations except for feelings of normalization versus alienation, perhaps because Mexican patients might not perceive the fact of feeling “weird” or different as something that generates emotional discomfort, a finding different from what has been reported in other cultures (TenHouten, 2017).
Among the limitations of the present study, it may be necessary to evaluate the stability of the instrument over time, to include patients undergoing psychological treatment, increase the number of participants, and including more men in the sample so that there is sex equivalence in future studies to increase the internal validity of the scale.
We suggest using this scale with patients at various stages such as diagnosis, treatment, follow-up and survival to consider possible medical and psychological treatments, as has been done in previous studies (Penedo et al., 2004, 2006; Yanez et al., 2015).
Conclusions
The Measurement of Current Status Scale (MOCS) in Mexican cancer patients has a factorial structure similar to the original version. It also obtained acceptable psychometric properties in part A and part B with lower indicators, as well as acceptable concurrent validity. With the above results we now have a first valid version that can be used with the Hispanic population, to monitor stress levels specifically in the oncology health setting.
References:
Almanza, J. de J., Juárez, I. R., & Pérez, S. (2008). Traducción, adaptación y validación del termómetro de distrés en una muestra de pacientes mexicanos con cáncer. Revista de Sanidad Militar, 62(5), 209-217.
American Psychological Association. (2020a). Assertiveness. APA Dictionary of Psychology. https://dictionary.apa.org/assertiveness
American Psychological Association. (2020b). Normality. APA Dictionary of Psychology. https://dictionary.apa.org/normality
American Psychological Association. (2020c). Alienation. APA Dictionary of Psychology. https://dictionary.apa.org/alienation
American Psychological Association. (2020d). Group cohesion. Dictionary of Psychology. https://dictionary.apa.org/group-cohesion
Antoni, M. H., Lechner, S. C., Kazi, A., Wimberly, S. R., Sifre, T., Urcuyo, K. R., Phillips, K., Glück, S., & Carver, C. S. (2006). How stress management improves quality of life after treatment for breast cancer. Journal of Consulting and Clinical Psychology, 74(6), 1143-1152. https://doi.org/10.1037/0022-006x.74.6.1152
Bleiker, E. M. A., Pouwer, F., Van Der Ploeg, H. M., Leer, J. W. H., & Adèr, H. J. (2000). Psychological distress two years after diagnosis of breast cancer: Frequency and prediction. Patient Education and Counseling, 40(3), 209-217. https://doi.org/10.1016/S0738-3991(99)00085-3
Byrne, B. M. (2010). Structural equation modeling with AMOS: Basic concepts, applications, and programming. Routledge/Taylor & Francis Group.
Carretero-Dios, H. & Pérez, C. (2005). Normas para el desarrollo y revisión de estudios instrumentales. International Journal of Clinical and Health Psychology, 5(3), 521-551.
Carver, C. S. (2006). Measure of Current Status (MOCS). Department of Psychology, University of Miami. http://www.psy.miami.edu/faculty/ccarver/sclMOCS.html.
Chhikara, B. S. & Parang, K. (2023). Global Cancer Statistics 2022: The trends projection analysis. Chemical Biology Letters, 10(1), 451.
Dai, S., Mo, Y., Wang, Y., Xiang, B., Liao, Q., Zhou, M., Li, X., Li, Y., Xiong, W., Li, G., Guo, C., & Zeng, Z. (2020). Chronic stress promotes cancer development. In Frontiers in Oncology, 10, 1492). https://doi.org/10.3389/fonc.2020.01492
Dobson, K. S. & Dozois, D. J. A. (2010). Historical and philosophical bases of the cognitive-behavioral therapies. In K. S. Dobson (Ed.), Handbook of cognitive-behavioral therapies (3rd ed., pp. 3-38). Guilford Press.
Fernández Seara, J. L. & Nielgo Robles, M. (1996, January). Escala de apreciación del estrés. TEA Ediciones S.A. https://www.ulima.edu.pe/pregrado/psicologia/gabinete-psicometrico/eae-escala-de-apreciacion-del-estres
Golden-Kreutz, D. M. & Andersen, B. L. (2004). Depressive symptoms after breast cancer surgery: Relationships with global, cancer-related, and life event stress. Psycho-Oncology, 13(3), 211-220. https://doi.org/10.1002/pon.736
Hair, J. F., Anderson, R. E., Tatham, R. L., & Black, W. C. (1999). Análisis Multivariante (5th ed.). Prentice-Hall.
Haugland, T., Wahl, A. K., Hofoss, D., & DeVon, H. A. (2016). Association between general self-efficacy, social support, cancer-related stress and physical health-related quality of life: A path model study in patients with neuroendocrine tumors. Health and Quality of Life Outcomes, 14(1), 11. https://doi.org/10.1186/s12955-016-0413-y
Holland, J. C., Andersen, B., Breitbart, W., & Buchmann, L. O. (2013). NCCN Clinical Practice Guidelines in Ocology Distress Management. National Comprehensive Cancer Network.
Horowitz, M., Wilner, N., & Alvarez, W. (1979). Impact of event scale: A measure of subjective stress. Psychosomatic Medicine, 41(3), 209-218. https://doi.org/10.1097/00006842-197905000-00004
Kang, D.-H., Park, N.-J., & McArdle, T. (2012). Cancer-specific stress and mood disturbance: Implications for symptom perception, quality of life, and immune response in women shortly after diagnosis of breast cancer. ISRN Nursing, 2012, 1-7. https://doi.org/10.5402/2012/608039
Kline, R. B. (2016). Principles and Practice of Structural Equation Modeling: Fourth Edition. The Guilford Press.
Lazarus, R. S. & Folkman, S. (1984). Stress, coping and adaptation. Springer.
Levenstein, S., Prantera, C., Varvo, V., Scribano, M. L., Berto, E., Luzi, C., & Andreoli, A. (1993). Development of the perceived stress questionnaire: A new tool for psychosomatic research. Journal of Psychosomatic Research, 37(1), 19-32. https://doi.org/10.1016/0022-3999(93)90120-5
Manzano Patiño, A. P. (2017). Introducción a los modelos de ecuaciones estructurales | Revista Investigación en Educación Médica. Investigación En Educación Médica, 7(25), 67-72.
Mora, J., Bautista, N., Natera, G., & Pedersen, D. (2013). Adaptación cultural de instrumentos de medida sobre estigma y enfermedad mental en la Ciudad de México. Salud Mental, 36(1), 9-18. https://doi.org/10.17711/sm.0185-3325.2013.002
Moreno-Smith, M., Lutgendorf, S. K., & Sood, A. K. (2010). Impact of stress on cancer metastasis. Future Oncology, 6(12), 1863-1881. https://doi.org/10.2217/fon.10.142
Papastavrou, E., Efstathiou, G., & Charalambous, A. (2011). Nurses’ and patients’ perceptions of caring behaviours: Quantitative systematic review of comparative studies. Journal of Advanced Nursing, 67(6), 1191-1205. https://doi.org/10.1111/j.1365-2648.2010.05580.x
Penedo, F. J., Dahn, J. R., Molton, I., Gonzalez, J. S., Kinsinger, D., Roos, B. A., Carver, C. S., Schneiderman, N., & Antoni, M. H. (2004). Cognitive-behavioral stress management improves stress-management skills and quality of life in men recovering from treatment of prostate carcinoma. Cancer, 100(1), 192-200. https://doi.org/10.1002/cncr.11894
Penedo, F. J., Molton, I., Dahn, J. R., Shen, B. J., Kinsinger, D., Traeger, L., Siegel, S., Schneiderman, N., & Antoni, M. (2006). A randomized clinical trial of group-based cognitive-behavioral stress management in localized prostate cancer: Development of stress management skills improves quality of life and benefit finding. Annals of Behavioral Medicine, 31(3), 261-270. https://doi.org/10.1207/s15324796abm3103_8
Phillips, K. M., Jim, H. S. L., Small, B. J., Tanvetyanon, T., Roberts, W. S., & Jacobsen, P. B. (2012). Effects of self-directed stress management training and home-based exercise on stress management skills in cancer patients receiving chemotherapy. Stress and Health, 28(5), 368-375. https://doi.org/10.1002/smi.2450
Pomery, E. A., Gibbons, F. X., & Stock, M. L. (2012). Social Comparison. In Encyclopedia of Human Behavior: Second Edition (pp. 463-469). Elsevier. https://doi.org/10.1016/B978-0-12-375000-6.00332-3
Roth, A. J., Kornblith, A. B., Batel-Copel, L., Peabody, E., Scher, H. I., & Holland, J. C. (1998). Rapid screening for psychologic distress in men with prostate carcinoma: A pilot study. Cancer, 82(10), 1904-1908. https://doi.org/10.1002/(sici)1097-0142(19980515)82:10%3C1904::aid-cncr13%3E3.0.co;2-x
Ruiz Fernández, M. Á., Díaz García, M. I., & Villalobos Crespo, A. (2012). Manual de Técnicas de Intervención Cognitivo Conductuales. Desclée De Brouwer.
Skinner, E. A. & Zimmer-Gembeck, M. (2016). Coping. In Encyclopedia of Mental Health: Second Edition (pp. 350-357). Elsevier. https://doi.org/10.1016/B978-0-12-397045-9.00036-7
Sociedad Mexicana de Oncología. (2016). Prevención y diagnóstico oportuno de cáncer. https://www.smeo.org.mx/descargables/COPREDOC_GUIA.pdf
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., & Bray, F. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 71(3). https://doi.org/10.3322/caac.21660
Taber, K. S. (2018). The use of Cronbach’s Alpha when developing and reporting research instruments in science education. Research in Science Education, 48(6), 1273-1296. https://doi.org/10.1007/s11165-016-9602-2
TenHouten, W. D. (2017). Self-estrangement and despair: Theorizing the affective basis of a variety of alienation. In Routledge advances in sociology. Alienation and affect. (pp. 91-104). Routledge/Taylor & Francis Group.
Yanez, B., McGinty, H. L., Mohr, D. C., Begale, M. J., Dahn, J. R., Flury, S. C., Perry, K. T., & Penedo, F. J. (2015). Feasibility, acceptability, and preliminary efficacy of a technology-assisted psychosocial intervention for racially diverse men with advanced prostate cancer. Cancer, 121(24), 44074415. https://dx.doi.org/10.1002/cncr.29658
Funding: This research project was funded by the National Council of Science and Technology (Consejo Nacional de Ciencia y Tecnología), support 720632, grant number 697234 for doctoral studies.
Data availability: The dataset supporting the results of this study is not available.
How to cite: Espinoza Bello, M., Galindo Vázquez, O., Penedo, F. J., Jiménez Ríos, M. Á., Ortega Andeane, P., Scavuzzo, A., García Méndez, M., & Meneses-García, A. (2023). Psychometric properties of the Measurement of Current Status (MOCS) Scale in Mexican cancer patients. Ciencias Psicológicas, 17(2), e-3009. https://doi.org/10.22235/cp.v17i2.3009
Authors’ participation: a) Conception and design of the work; b) Data acquisition; c) Analysis and interpretation of data; d) Writing of the manuscript; e) Critical review of the manuscript.
M. E. B. has contributed in a, b, c, d, e; O. G. V. in a, b, c, d, e; F. J. P. in d, e; M. A. J. R. in d, e; P. O. A. in d, e; A. S. in e; M. G. M. in d, e; A. M.-G. in a, e.
Scientific editor in-charge: Dra. Cecilia Cracco.